Corneal Distortion and Corneal Morphological Parameters in Naïve Eyes Analyzed with a Scheimpflug Camera
Abstract
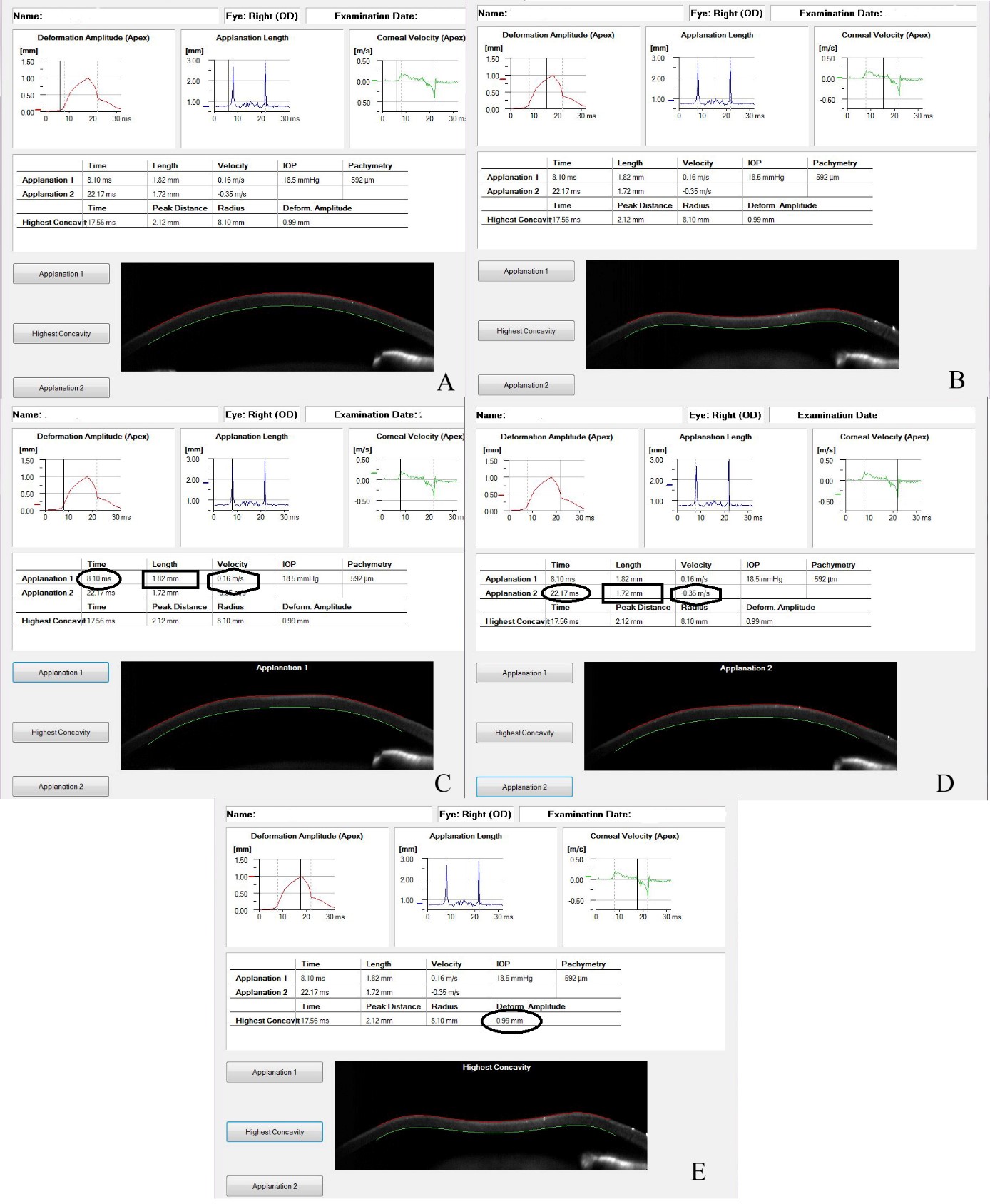
Background: The study of the corneal biomechanical properties (CBP) is gaining always more interest, thanks to the applications to refractive surgery and to the overall management of several corneal diseases.
Purpose: To analyze the eventual relationships between corneal distortion and morphologic features in healthy subjects.
Methods: one eye of one hundred and fifty-two healthy participants, 87 women and 65 men, aging from 23 to 65 years old, were evaluated in this study. Every eye underwent a complete clinical examination, that included also a tomographic scan using Pentacam HR (Oculus, Wetzlar, Germany) and a biomechanical evaluation using Corvis ST (Oculus, Wetzlar, Germany). Linear regressions among refractive defect, corneal volume (CV), anterior corneal curvature and central corneal thickness (CCT) vs corneal biomechanical features provided by Corvis ST have been ran using SPSS software version 18.0.
Results: Corneal distortion factors showed a low correlation both with corneal morphological parameters and with refractive defect. No significant correlations (p> 0.01) were found among morphologic and biomechanical features evaluated.
Discussion: results observed in this study could help in recognize the healthy range of values of CBP parameters provided by CST. This information could be very useful in many ophthalmology topics such as the accurate IOP measurement, the early diagnosis of corneal degenerations, such as keratoconous, and the screening of subject undergoing refractive surgery.
Conclusions: even if data of this study need to be confirmed in further ones with larger populations, results here observed suggest that Corvis ST is a device providing an evaluation of corneal distortion not influenced by morphological corneal factors. This information could help in better screening and managing the diseased corneas.
References
[2] Abd, E. M. S., Elsobky, H. M., Zaky, A. G., Hassan, E. A. M., & Khalaf, Allah, M. T. (2019). Corneal biomechanics and intraocular pressure assessment after penetrating keratoplasty for non keratoconic patients, long term results. BMC Ophthalmol, 19, 172. https://doi.org/10.1186/s12886-019-1186-y
[3] Koprowski, R., & Wilczyński, S. (2018). Corneal vibrations during intraocular pressure measurement with an air-puff method. J. Healthc. Eng, 11, 5705749. https://doi.org/10.1155/2018/5705749
[4] Guo, H., Hosseini-Moghaddam, S. M., & Hodge, W. (2019). Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis. BMC Ophthalmol, 19, 167. https://doi.org/10.1186/s12886-019-1165-3
[5] Lanza, M., Iaccarino, S., & Bifani, M. (2016). In vivo human corneal deformation analysis with a Scheimpflug camera, a critical review. J. Biophotonics, 9, 464-477. https://doi.org/10.1002/jbio.201500233
[6] Luce, D. A. (2005). Determining in vivo biomechanical properties of the cornea with an ocular response analyser. J. Cataract. Refract. Surg, 31, 156-162. https://doi.org/10.1016/j.jcrs.2004.10.044
[7] Hong, J., Xu, J., Wei, A., Deng, S. X., Cui, X., Yu, X. et al. (2013). A new tonometer--the Corvis ST tonometer: clinical comparison with noncontact and Goldmann applanation tonometers. Invest. Ophthalmol. Vis. Sci, 54, 659-665. https://doi.org/10.1167/iovs.12-10984
[8] Lanza, M., Cennamo, M., Iaccarino, S., Romano, V., Bifani, M., Irregolare, C. et al. (2015). Evaluation of corneal deformation analysed with a Scheimpflug based device. Cont. Lens. Anterior Eye, 38, 89-93 https://doi.org/10.1016/j.clae.2014.10.002
[9] Ma, J., Wang, Y., Wei, P., & Jhanji, V. (2018). Biomechanics and structure of the cornea: implications and
association with corneal disorders. Surv. Ophthalmol, 63, 851-861. https://doi.org/10.1016/j.survophthal.2018.05.004
[10] Hong, J., Xu, J., Wei, A., Deng, S. X., Cui, X., Yu, X. et al. (2013). A New Tonometer-The Corvis ST Tonometer: Clinical Comparison with Noncontact and Goldmann Applanation Tonometers. Invest. Ophthalmol. Vis. Sci, 54, 659-665. https://doi.org/10.1167/iovs.12-10984
[11] Hon, Y., & Lam, A. K. (2013). Corneal deformation measurement using scheimpflug noncontact tonometry. Optom. Vis. Sci, 90, e1-8. https://doi.org/10.1097/OPX.0b013e318279eb87
[12] Huseynova, T., Abdulaliyeva, F., & Lanza, M. (2016). Comparison of Scheimpflug imaging parameters between steep and keratoconic corneas of Caucasian eyes. Clin. Ophthalmol, 10, 603-608. https://doi.org/10.2147/OPTH.S102683
[13] Lanza, M., Iaccarino, S., Mele, L., Carnevale, U. A., Irregolare, C., Lanza, A. et al. (2016). Intraocular pressure evaluation in healthy eyes and diseased ones using contact and non contact devices. Cont. Lens. Anterior Eye, 39, 154-159. https://doi.org/10.1016/j.clae.2015.10.001
[14] Miki, A., Maeda, N., Ikuno, Y., Asai, T., Hara, C., & Nishida, K. (2017). Factors associated with corneal deformation responses measured with a dynamic Scheimpflug analyzer. Invest. Ophthalmol. Vis. Sci, 58, 538-544. https://doi.org/10.1167/iovs.16-21045
[15] Miki, A., Yasukura, Y., Weinreb, R. N., Yamada, T., Koh, S., Asai, T. et al. (2019). Dynamic Scheimpflug ocular biomechanical parameters in healthy and medically controlled glaucoma eyes. J. Glaucoma, 28, 588-592. https://doi.org/10.1097/IJG.0000000000001268
[16] Fuchsluger, T. A., Brettl, S., Geerling, G., Kaisers, W., & Franko, Zeitz, P. (2019). Biomechanical assessment of healthy and keratoconic corneas (with/without crosslinking) using dynamic ultrahigh-speed Scheimpflug technology and the relevance of the parameter (A1L-A2L). Br. J. Ophthalmol. 103, 558-564.
https://doi.org/10.1136/bjophthalmol-2017-311627
[17] Herber, R., Ramm, L., Spoerl, E., Raiskup, F., Pillunat, L. E., & Terai, N. (2019). Assessment of corneal biomechanical parameters in healthy and keratoconic eyes using dynamic bidirectional applanation device and dynamic Scheimpflug analyzer. J. Cataract Refract. Surg, 45, 778-788. https://doi.org/10.1016/j.jcrs.2018.12.015
[18] Zhang, Y., Wang, Y., Li, L., Dou, R., Wu, W., Wu, D. et al. (2018). Corneal stiffness and its relationship with other corneal biomechanical and nonbiomechanical parameters in myopic eyes of Chinese patients. Cornea, 37, 881-885. https://doi.org/10.1097/ICO.0000000000001605
[19] Salouti, R., Bagheri, M., Shamsi, A., & Zamani M. (2020). Corneal parameters in healthy subjects assessed by Corvis ST. J. Ophthalmic Vis. Res,. 15, 24‐31. https://doi.org/10.18502/jovr.v15i1.5936
[20] Garcia-Feijoo, J., Martinez-de-la-Casa, J. M., Morales-Fernandez, L., Saenz-Frances, F., Santos-Bueso, E., Sofia, Garcia-Saenz, S. et al. (2015). New technologies for measuring intraocular pressure. Prog Brain Res, 221, 67‐79. https://doi.org/10.1016/bs.pbr.2015.06.003
[21] Jędzierowska, M., & Koprowski, R. (2019). Novel dynamic corneal response parameters in a practice use: a critical review. Biomed. Eng. Online, 18, 17. https://doi.org/10.1186/s12938-019-0636-3

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)