Screening, Sensitivity, Specificity, and So Forth: A Second, Somewhat Skeptical, Sequel
Abstract
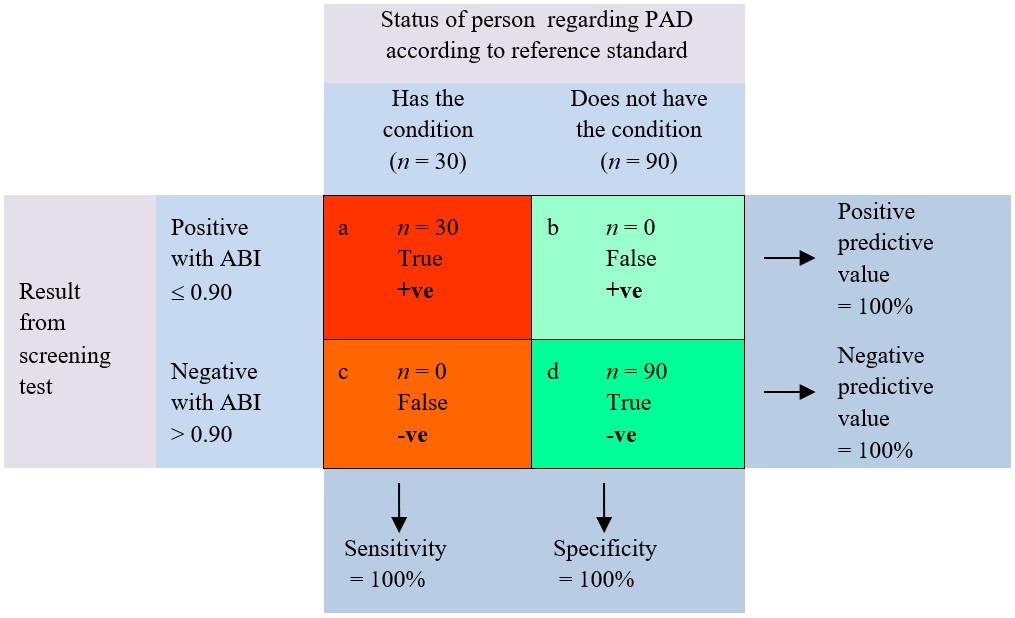
This article is concerned with the sensitivity, specificity, predictive values, and other metrics associated with screening tests. It has direct origins in two previous articles. In this third article, the author of the first article writes about topics and issues that were addressed only minimally in his previous article and expands on topics raised by authors of the second article. In particular, attention is turned to wording and terminology that can be idiosyncratic and confusing with regard to screening versus diagnosis as well as to issues associated with reference (“gold”) standards and screening tests, and to the importance of cutpoints and prevalence in relation to metrics associated with screening tests. The primary aims are to help readers attain clarity about topics that they might have felt unsure about; gain reassurance about conceptual difficulties in the field that, once recognized for what they are, can become less problematic because it is possible to be confident about not being confident; and, where appropriate, adopt an appropriately skeptical attitude about screening tests and their associated metrics. Examples are drawn from the use of ankle–brachial and toe–brachial indices for identifying peripheral artery disease, although wider applicability is intended.
References
Akobeng, A. K. (2006). Understanding diagnostic tests 1: Sensitivity, specificity and predictive values. Acta Paediatrica, 96, 338–341. https://doi.org/10.1111/j.1651-2227.2006.00180
Al Fattani, A. A., & Aljoudi, A. (2015). Sources of bias in diagnostic accuracy studies. Journal of Applied Hematology, 6, 178–180. https://doi.org/10.4103/1658-5127.171991
Al-Qaisi, M., Nott, D. M., King, D. H., & Kaddoura, S. (2009). Ankle brachial pressure index (ABPI): An update for practitioners. Vascular Health and Risk Managment, 5, 833–841. https://doi.org/10.2147/VHRM.S6759
Bhamidipaty, V., Dean, A., Yap, S. L., Firth, J., Barron, M., Allard, B., & Chan, S. T. F. (2015). Second toe systolic pressure measurements are valid substitutes for first toe systolic pressure measurements in diabetic patients: A prospective study. European Journal of Vascular and Endovascular Surgery, 49, 77–82. https://doi.org/10.1016/j.ejvs.2014.09.011
Bonham, P. A. (2011). Measuring toe pressures using a portable photoplethysmograph to detect arterial disease in high risk patients: An overview of the literature. Ostomy Wound Management, 57, 36–44. https://www.o-wm
.com/files/owm/pdfs/OWM_November2011_Bonham.pdf
Bossuyt, P. M., Reitsma, J. B., Bruns D. E., Gatsonis, C. A., Glasziou, P. P., Irwig, L. M., … de Vet, H. C. W. (2003). Towards complete and accurate reporting of studies of diagnostic accuracy: The STARD initiative. Clinical Chemistry, 49, 1–6. https://doi.org/10.1373/49.1.1
Brenner, H., & Gefeller, O. (1997). Variation of sensitivity, specificity, likelihood ratios and predictive values with disease prevalence. Statistics in Medicine, 16, 981–991. https://doi.org/10.1002/(SICI)1097-0258(19970515)16:9<981::AID-SIM510>3.0.CO;2-N
Bundó, M., Urrea, M., Muñoz, L., Llussà, J., Forés, R., & Torán, P. (2013). [Correlation between toe-brachial index and ankle-brachial index in patients with diabetes mellitus type 2]. Medicina Clinica (Barc), 140, 390–394. Spanish. https://doi.org/10.1016/j.medcli.2012.03.012
Cadogan, A., McNair, P., Laslett, M., & Hing, W. (2013). Shoulder pain in primary care: Diagnostic accuracy of clinical examination tests for non-traumatic acromioclavicular joint pain. BMC Musculoskeletal Disorders, 14, 156–166. https://doi.org/10.1186/1471-2474-14-156
Cadogan, A., McNair, P., Laslett, M., Hing, W., & Taylor, S. (2013). Diagnostic accuracy of clinical examination features for identifying large rotator cuff tears in primary health care. Journal of Manual and Manipulative Therapy, 21, 148–159. https://doi.org/10.1179/2042618612Y.0000000020
Campbell, N., Chockalingam, A., Fodor, J. G., & McKay, D. W. (1990). Accurate, reproducible measurement of blood pressure. Canadian Medical Association Journal, 143, 19–24. https://www.ncbi.nlm.nih.gov/pmc
/articles/PMC1452062/
Cardenas, V., Seo, K., Sheth, S., & Meyr, A. J. (2018). Prevalence of lower-extremity arterial calcification in patients with diabetes mellitus complicated by foot disease at an urban US tertiary-care center. Journal of the American Podiatric Medical Association, 108, 267–271. https://doi.org/10.7547/16-075
Caro, J., Migliaccio-Walle, K., Ishak, K., & Proskorovsky, I. (2005). The morbidity and mortality following a diagnosis of peripheral arterial disease: Long-term follow-up of a large database. BMC Cardiovascular Disorders, 5, 14. https://www.ncbi.nlm.nih.gov/pubmed/15972099
Caruana, M. F., Bradbury, A. W., & Adam, D. (2005). The validity, reliability, reproducibility and extended utility of ankle to brachial pressure index in current vascular surgical practice. European Journal of Vascular and Endovascular Surgery, 29, 443–451. https://doi.org/10.1016/j.ejvs.2005.01.015
Chen, J., Mohler, E. R. 3rd, Garimella, P. S., Hamm, L. L., Xie, D., Kimmel, S., Townsend, R. R., … He, J. (2016). Ankle brachial index and subsequent cardiovascular disease in patients with chronic kidney disease. Journal of the American Heart Association, 5(6), pii:e003339. https://doi.org/10.1161/JAHA.116.003339
Chongthawonsatid, S., & Dutsadeevettakul, S. (2017). Validity and reliability of the ankle-brachial index by oscillometric blood pressure and automated ankle-brachial index. Journal of Research in Medical Science, 22, 44. https://doi.org/10.4103/jrms.JRMS_728_16
Coulthard, M. G. (2007). Quantifying how tests reduce diagnostic uncertainty. Archives of Disease in Childhood, 92, 404–408. https://doi.org/10.1136/adc.2006.111633
Criqui, M. H., & Aboyans, V. (2015). Epidemiology of peripheral artery disease. Circulation Research, 116, 1509–1526. https://www.ahajournals.org/doi/abs/10.1161/CIRCRESAHA.116.303849?url_ver=Z39.88-2003&rfr
_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed&
Criqui, M. H., McClelland, R. L., McDermott, M. M., Allison, M. A., Blumenthal, R. S., Aboyans V., … Shea S. (2010). The ankle-brachial index and incident cardiovascular events in the MESA (Multi-Ethnic Study of Atherosclerosis). Journal of the American College of Cardiology, 56, 1506–1512. https://doi.org/10.1016/j.jacc.2010.04.060
European Stroke Organisation, Tendera, M., Aboyans, V., Bartelink, M. L., Baumgartner, I., Clément, D., … Van Damme, H. (2011). ESC guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: The Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). European Heart Journal, 32, 2851–2906. https://doi.org/10.1093/eurheartj/ehr211
Formosa, C., Ellul, C., Mizzi, A., Mizzi, S., & Gatt, A. (2018). Interrater reliability of spectral Doppler waveform analysis among podiatric clinicians. Journal of the American Podiatric Medical Association, 108, 280–284. https://doi.org/10.7547/16-026
Goehring, C., Perrier, A., & Morabia, A. (2004). Spectrum bias: A quantitative and graphical analysis of the variability of medical diagnostic test performance. Statistics in Medicine, 23, 125–135. https://www.ncbi.nlm
.nih.gov/pubmed/14695644
Goldstein, L. N., Wells, M., & Sliwa, K. (2014). Blood pressure measurements in the ankle are not equivalent to blood pressure measurements in the arm. South African Medical Journal, 104, 869–873. https://doi.org/10.7196/SAMJ.8102
Gong, Y., Cao, K. W., Xu, J. S., Li, J. X., Hong, K., Cheng, X. S., & Su, H. (2015). Valuation of normal range of ankle systolic blood pressure in subjects with normal arm systolic blood pressure. PLoS One., 10(6), e0122248. https://doi.org/10.1371/journal.pone.0122248
Gornik, H. L. (2009). Rethinking the morbidity of peripheral arterial disease and the “normal” ankle-brachial index. Journal of the American College of Cardiology, 53, 1063–1064. https://doi.org/10.1016/j.jacc.2008.12.019
Grunau, G. L., & Linn, S. (2018). Commentary: Sensitivity, specificity, and predictive values: Foundations, pliabilities, and pitfalls in research and practice. Frontiers in Public Health, 6, Article 256. https://doi.org/10.3389/fpubh.2018.00256
Hinchliffe, R. J., Brownrigg, J. R. W., Apelqvist, J., Boyko, E. J., Fitridge, R., Mills, J. L., … Schaper, N. C. (2016). IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Diabetes Metabolism Research Reviews, 32(Suppl 1), 37–44. https://doi.org/10.1002/dmrr.2698
Høyer, C., Sandermann, J., & Petersen, L. J. (2013). The toe-brachial index in the diagnosis of peripheral arterial disease. Journal of Vascular Surgery, 58, 231–238. https://doi.org/10.1016/j.jvs.2013.03.044
Irving, G., & Holden, J. (2013). The time-efficiency principle: Time as the key diagnostic strategy in primary care. Family Practice, 30, 386–389. https://doi.org/10.1093/fampra/cmt007
Ix, J. H., Miller, R. G., Criqui, M. H., & Orchard, T. J. (2012). Test characteristics of the ankle-brachial index and ankle-brachial difference for medial arterial calcification on X-ray in type 1 diabetes. Journal of Vascular Surgery, 56, 721–727. https://doi.org/10.1016/j.jvs.2012.02.042
Jelinek, H. F., & Austin, M. (2006). The ankle–brachial index in clinical decision making. Foot (Edinb), 16, 153–157. https://doi.org/10.1016/j.foot.2006.04.003
Jönelid, B., Johnston, N., Berglund, L., Andrén, B., Kragsterman, B., & Christersson, C. (2016). Ankle brachial index most important to identify polyvascular disease in patients with non-ST elevation or ST-elevation myocardial infarction. European Journal of Internal Medicine, 30, 55–60. https://doi.org/10.1016/j.ejim
.2015.12.016
Kesson, A. M. (2009). Predictive values, sensitivity and specificity in clinical virology. Retrieved June 8, 2019 from http://www.virologyresearch.unsw.edu.au/virology/wp-content/uploads/2013/08/VIM09
_AlisonKesson_ClinicalVirology.pdf
Lalkhen, A. G., & McCluskey, A. (2008). Clinical tests: Sensitivity and specificity. Continuing Education in Anaesthesia Critical Care & Pain, 8, 221–223. https://doi.org/10.1093/bjaceaccp/mkn041
Leeflang, M. M., Bossuyt, P. M., & Irwig, L. (2009). Diagnostic test accuracy may vary with prevalence: Implications for evidence-based diagnosis. Journal of Clinical Epidemiology, 62, 5–12. https://doi.org/10.1016/j.jclinepi.2008.04.007
Lewis, J. E. A., Williams, P., & Davies, J. H. (2016). Non-invasive assessment of peripheral arterial disease: Automated ankle brachial index measurement and pulse volume analysis compared to duplex scan. SAGE Open Medicine, 4. https://doi.org/10.1177/2050312116659088
Li, J., & Fine, J. P. (2011). Assessing the dependence of sensitivity and specificity on prevalence in meta-analysis. Biostatistics, 12, 710–722. https://doi.org/10.1093/biostatistics/kxr008
Loong, T. W. (2003). Understanding sensitivity and specificity with the right side of the brain. BMJ., 327, 716–719. https://doi.org/10.1136/bmj.327.7417.716
Manrai, A. K., Bhatia, G., Strymish, J., Kohane, I. S., & Jain, S. H. (2014). Medicine's uncomfortable relationship with math: Calculating positive predictive value. JAMA Internal Medicine, 174, 991–993. https://doi.org/10.1001/jamainternmed.2014.1059
Mätzke, S., Franckena, M., Albäck, A., Railo, M., & Lepäntalo, M. (2003). Ankle brachial index measurements in critical leg ischaemia – The influence of experience on reproducibility. Scandinavian Journal of Surgery, 92, 144–147. https://doi.org/10.1177/145749690309200206
McAra, S. (2015). Glyceryl trinitrate and toe–brachial indexes in pedal ischaemia. (Unpublished doctoral dissertation). Charles Sturt University. Albury, NSW, Australia. Retrieved from https://researchoutput.csu.edu.au/en/publications/glyceryl-trinitrate-and-toe-brachial-indexes-in-pedal
-ischaemia-3
McAra, S., & Trevethan, R. (2018). Measurement of toe-brachial indices in people with subnormal toe pressures: Complexities and revelations. Journal of the American Podiatric Medical Association, 108, 115–125. https://doi.org/10.7547/16-036
McAra, S., Trevethan, R., Wang, L., & Tinley, P. (2017). Vascular screening of the foot: For life and limb. Diabetes and Primary Care Australia, 2(1), 16–24. http://pcdsa.com.au/wp-content/uploads/2016/12/DPCA2-1_16%E2%80%9324_wm.pdf
McHugh, M. L. (2012). Interrater reliability: The kappa statistic. Biochemia Medica (Zagreb), 22, 276–282. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900052/
Mills, J. L. Sr, Conte, M. S., Armstrong, D. G., Pomposelli, F. B., Schanzer, A., Sidawy, A. N., & Andros, G. (2014). The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: Risk stratification based on wound, ischemia, and foot infection (WIfI). Journal of Vascular Surgery, 59, 220–234. e1-2. https://doi.org/10.1016/j.jvs.2013.08.003
Molinaro, A. M. (2015). Diagnostic tests: How to estimate the positive predictive value. Neuro-Oncology Practice, 2, 162–166. https://doi.org/10.1093/nop/npv030
Mulherin, S. A., & Miller W. C. (2002). Spectrum bias or spectrum effect? Subgroup variation in diagnostic test evaluation. Annals of Internal Medicine, 137, 598–602. https://www.ncbi.nlm.nih.gov/pubmed/12353947
Nishimura, H., Miura, T., Minamisawa, M., Ueki, Y., Abe, N., Hashizume, N., … Kuwahara, K. (2016). Clinical characteristics and outcomes of patients with high ankle-brachial index from the IMPACT-ABI study. PLoS ONE, 11(11), e0167150. https://doi.org/10.1371/journal.pone.0167150
Nunnally, J. C., & Bernstein, I. H. (1994). Psychometric theory (3rd ed.). New York, NY: McGraw Hill.
Okada, R., Yasuda, Y., Tsushita, K., Wakai, K., Hamajima, N., & Matsuo, S. (2015). Within-visit blood pressure variability is associated with prediabetes and diabetes. Scientific Reports, 5, Article number 7964. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295087/
Okamoto, K., Oka, J., Maesato, K., Ikee, R., Mano, T., Moriya, H., … Kobayashi, S. (2006). Peripheral arterial occlusive disease is more prevalent in patients with hemodialysis: Comparison with findings of multidetector-row computed tomography. American Journal of Kidney Diseases, 48, 269–276. https://doi.org/10.1053/j.ajkd.2006.04.075
Påhlsson, H. I., Laskar, C., Stark, K., Andersson, A., Jogestrand, T., & Wahlberg, E. (2007). The optimal cuff width for measuring toe blood pressure. Angiology, 58, 472–476. https://doi.org/10.1177/0003319706294606
Parati, G., Ochoa, J. E., Salvi, P., Lombardi, C., & Bilo, G. (2013). Prognostic value of blood pressure variability and average blood pressure levels in patients with hypertension and diabetes. Diabetes Care, 36(Supplement 2), S312-S324. https://doi.org/10.2337/dcS13-2043
Parikh, R., Mathai, A., Parikh, S., Sekhar, G. C., & Thomas, R. (2008). Understanding and using sensitivity, specificity and predictive values. Indian Journal of Ophthalmology, 56, 45–50. https://doi.org/10.4103/0301
-4738.37595
Pérez-Martin, A., Meyer, G., Demattei, C., Böge, G., Laroche, J-P., Quéré, I., & Dauzat, M. (2010). Validation of a fully automatic photoplethysmographic device for toe blood pressure measurement. European Journal of Vascular and Endovascular Surgery, 40, 515–520. https://doi.org/10.1016/j.ejvs.2010.06.008
Pewsner, D., Battaglia, M., Minder, C., Marx, A., Bucher, H. C., & Egger, M. (2004). Ruling a diagnosis in or out with “SpPIn” and “SnNOut”: A note of caution. BMJ, 329, 209–213. https://doi.org/10.1136/bmj.329.7459
.209
Portney, L. G., & Watkins, M. P. (2009). Foundations of clinical research: Applications to practice (3rd. ed). Upper Saddle River, NJ: Pearson Education.
Puhan, M. A., Steurer, J., Bachmann, L. M., & ter Riet, G. (2005). A randomized trial of ways to describe test accuracy: The effect on physicians’ post-test probability estimates. Annals of Internal Medicine, 143, 184–189. https://doi.org/10.7326/0003-4819-143-3-200508020-00004
Quong, W. L., Fung, A. T., Yu, R. Y., & Hsaing, Y. N. H. (2016). Reassessing the normal toe-brachial index in young healthy adults. Journal of Vascular Surgery, 63, 652–656. https://doi.org/10.1016/j.jvs.2015.09.019
Ray, P., Le Manach, Y., Riou, B., & Houle, T. T. (2010). Statistical evaluation of a biomarker. Anesthesiology, 112, 1023–1040. https://doi.org/10.1097/ALN.0b013e3181d47604
Reid, M. C., Lane, D. A., & Feinstein, A. R. (1998). Academic calculations versus clinical judgments, practicing physicians’ use of quantitative measures of test accuracy. American Journal of Medicine, 104, 374–380. https://doi.org/10.1016/S0002-9343(98)00054-0
Rich, K. (2015). Toe blood pressure and toe-brachial index. Journal of Vascular Nursing., 33, 164–166. https://doi.org/10.1016/j.jvn.2015.09.002
Romanos, M. T., Raspovic, A., & Perrin, B. M. (2010). The reliability of toe systolic pressure and the toe brachial index in patients with diabetes. Journal of Foot and Ankle Research, 3, 31. https://doi.org/10.1186/1757-1146
-3-31
Rooke, T. W., Hirsch, A. T., Misra, S., Sidawy, A. N., Beckman, J. A., Findeiss L. K., … Zierler, R. E. (2011). ACCF/AHA Focused update of the guideline for the management of patients with peripheral artery disease. Circulation, 124, 2020–2045. https://doi.org/10.1161/CIR.0b013e31822e80c3
Saunders, J. (2000). The practice of clinical medicine as an art and as a science. Medical Humanities, 26(1). https://doi.org/10.1136/mh.26.1.18
Sawka, A., & Carter, S. A. (1992). Effect of temperature on digital systolic pressures in lower limb in arterial disease. Circulation, 85, 1097–1101. https://doi.org/10.1161/01.CIR.85.3.1097
Schmidt, R. L., & Factor, R. E. (2013). Understanding sources of bias in diagnostic accuracy studies. Archives of Pathology and Laboratory Medicine, 137, 558–565. https://doi.org/10.5858/arpa.2012-0198-RA
Šimundić, A-M. (2009). Measures of diagnostic accuracy: Basic definitions. Electronic Journal of the International Federation of Clinical Chemistry and Laboratory Medicine, 19, 203–211. https://www.ncbi
.nlm.nih.gov/pubmed/27683318
Singh, S., Bailey, K. R., & Kullo, I. J. (2013). Ethnic differences in ankle brachial index are present in middle-aged individuals without peripheral arterial disease. International Journal of Cardiology, 162, 228–233. https://doi.org/10.1016/j.ijcard.2011.05.068
Sonter, J., Chuter, V., & Casey, S. (2015). Intratester and intertester reliability of toe pressure measurements in people with and without diabetes performed by podiatric physicians. Journal of the American Podiatric Medical Association., 105, 201–208. https://doi.org/10.7547/0003-0538-105.3.201
Sonter, J., Sadler, S., & Chuter, V. (2015). Inter-rater reliability of automated devices for measurement of toe systolic blood pressure and the toe brachial index. Blood Pressure Monitoring, 20, 47–51. https://doi.org/10.1097/MBP.0000000000000083
Sonter, J., Tehan, P., & Chuter, V. (2017). Toe brachial index measured by automated device compared to duplex ultrasonography for detecting peripheral arterial disease in older people. Vascular, 25, 612–617. https://doi.org/10.1177/1708538117705293
Steurer, J., Fischer, JE., Bachmann, LM., Koller, M., & ter Riet, G. (2002). Communicating accuracy of tests to general practitioners: A controlled study. BMJ, 324(7341), 824–826. https://doi.org/10.1136/bmj.324.7341
.824
Suominen, V., Rantanen, T., Vanermo, M., Saarinen, J., & Salenius J. (2008). Prevalence and risk factors of PAD among patients with elevated ABI. European Journal of Vascular and Endovascular Surgery, 35, 709–714. https://doi.org/10.1016/j.ejvs.2008.01.013
Suzuki, K. (2007). How to diagnose peripheral artery disease. Podiatry Today, 20(4), 54–65. http://www.podiatrytoday.com/article/6952
Tehan, P. E., Bray, A., & Chuter, V. H. (2016). Non-invasive vascular assessment in the foot with diabetes: Sensitivity and specificity of the ankle brachial index, toe brachial index and continuous wave Doppler for detecting peripheral arterial disease. Journal of Diabetes and its Complications, 30, 155–160. https://doi.org/10.1016/j.jdiacomp.2015.07.019Tehan, P. E., Santos, D., & Chuter, V. H. (2016). A systematic review of the sensitivity and specificity of the toe-brachial index for detecting peripheral artery disease. Vascular Medicine, 21, 382–389. https://doi.org/10.1177/1358863X16645854
Tehan, P., Bray, A., Keech, R., Rounsley, R., Carruthers, A., & Chuter, V. H. (2015). Sensitivity and specificity of the toe brachial index for detecting peripheral arterial disease: Initial findings. Journal of Ultrasound in Medicine, 34, 1737–1743. https://doi.org/10.7863/ultra.15.14.09071
Trevethan, R. (2017a). Intraclass correlation coefficients: Clearing the air, extending some cautions, and making some requests. Health Services Outcomes Research Methodology, 17, 127–143. https://doi.org/10.1007/s10742-016-0156-6
Trevethan, R. (2017b). Sensitivity, specificity, and predictive values: Foundations, pliabilities, and pitfalls in research and practice. Frontiers in Public Health, 5, Article 307. https://doi.org/10.3389/fpubh.2017.00307
Trevethan, R. (2018). Subjecting the ankle-brachial index to timely scrutiny: Is it time to say goodbye to the ABI? Scandinavian Journal of Clinical and Laboratory Investigation, 78, 94–101. https://doi.org/10.1080
/00365513.2017.1416665
Trevethan, R. (2019). Consistency of toe systolic pressures, brachial systolic pressures, and toe-brachial indices in people with and without diabetes. Current Diabetes Reviews, 15, 85–92. https://doi.org/10.2174
/1573399814666180123113619
Trevethan, R. (2019). Toe systolic pressures and toe-brachial indices: Uses, abuses, and shades of gray. Blood Pressure Monitoring, 24, 45–51. https://doi.org/10.1097/MBP.0000000000000372
Vetter, T. R., Schober P., & Mascha, E. J. (2018). Diagnostic testing and decision-making: Beauty is not just in the eye of the beholder. Anesthesia and Analgesia, 127, 1085–1091. https://doi.org/10.1213/ANE
.0000000000003698
Watanabe, Y., Masaki, H., Yunoki, Y., Tabuchi, A., Morita, I., Mohri, S., & Tanemoto, K. (2015). Ankle-brachial index, toe-brachial index, and pulse volume recording in healthy young adults. Annals of Vascular Diseases, 8, 227–235. https://doi.org/10.3400/avd.oa.15-00056
Whiting, P. F., Davenport, C., Jameson, C., Burke, M., Sterne, J. A. C., Hyde, C., & Ben-Shlomo, Y. (2015). How well do health professionals interpret diagnostic information? A systematic review. BMJ Open, 5(7), e008155. https://doi.org/10.1136/bmjopen-2015-008155
Whiting, P. F., Rutjes, A. W. S., Westwood, M. E., Mallett, S., Deeks, J. J., Reitsma, J. B., … QUADAS-2 Group. (2011). QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine, 155, 529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Willis, B. H. (2008). Spectrum bias—why clinicians need to be cautious when applying diagnostic test studies. Family Practice, 25, 390–396. https://doi.org/10.1093/fampra/cmn051
Wilson, J. M. G., & Jungner, G. (1968). Principles and practice of screening for disease. Geneva: World Health Organization. Retrieved from http://www.who.int/iris/handle/10665/37650
Wong, H. B., & Lim, G. H. (2011). Measures of diagnostic accuracy: Sensitivity, specificity, PPV and NPV. Proceedings of Singapore Healthcare, 40, 316–318. https://doi.org/10.1177/201010581102000411
Xu, D., Li, J., Zou, L., Xu, Y., Hu, D., Pagoto, S., & Ma, Y. (2010). Sensitivity and specificity of the ankle–brachial index to diagnose peripheral artery disease: A structured review. Vascular Medicine, 15, 361–369. https://doi.org/10.1177/1358863x10378376
Youden, W. J. (1950). Index for rating diagnostic tests. Cancer, 3, 32–35. https://doi.org/10.1002/1097-0142
(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3
Young, M. J., Adams, J. E., Anderson, G. F., Boulton, A. J. M., & Cavanagh, P. R. (1993). Medial arterial calcification in the feet of diabetic patients and matched non-diabetic control subjects. Diabetologia, 36, 615–621. https://doi.org/10.1007/BF00404070
Zhu, W., Zeng, N., & Wang, N. (2010). Sensitivity, specificity, accuracy, associated confidence interval and ROC analysis with Practical SAS® implementations. Retrieved June 7 2019, from http://www.lexjansen.com/nesug
/nesug10/hl/hl07.pdf

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)