The Application Value of CRRT in the Treatment of Cardio-Renal Syndrome: A Meta Analysis
Abstract
Objective: To evaluate the therapeutic effect of continuous renal replacement therapy (CRRT) combined with drug therapy and drug therapy alone on cardiorenal syndrome (CRS) by statistically comparing the efficacy of CRRT in the clinical treatment of CRS.
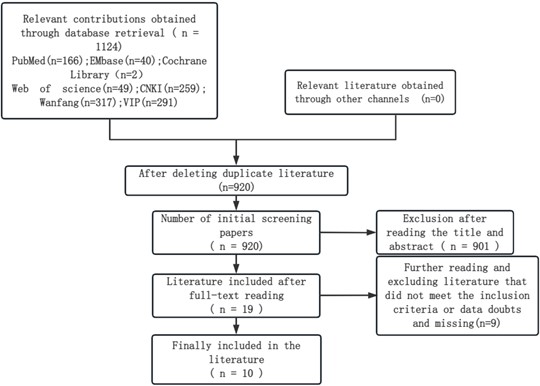
Method: Chinese databases (China National Knowledge Infrastructure, VIP Database, Wanfang Database) and English databases (PubMed, EmBase, The Cochrane Library, Web of Science) were searched for literature on continuous renal replacement therapy (CRRT) and the application of conventional drugs in cardiorenal syndrome (CRS) using computers. The search period was from the establishment of each database to September 1, 2023. By reading and screening the title, abstract, and full text, 10 articles that meet the inclusion criteria were finally included. Excel was used to summarize and integrate the data, and RevMan5.3 software was used for outcome indicator analysis.
Result: A total of 10 articles were included. Including 741 patients, including 369 patients in the continuous renal replacement therapy (CRRT) combined with drug treatment group and 372 patients in the internal medicine drug treatment group. 1. Cr: The decrease in CRRT group was higher than that in the internal medicine drug treatment group[MD=-58.73, 95%CI(-108.77, -8.69),P=0.02], (I²=98%, P<0.00001); 2. LVEF: The recovery of the CRRT group was better than that of the internal medicine drug treatment group [MD=5.93,95%CI(3.21, 8.65),P<0.0001],(I²=85%,P<0.00001); 3. BUN: The CRRT group showed better reduction than the internal medicine drug treatment group[MD=-1.21, 95%CI(-1.75, -0.67), P<0.0001], (I²=93%, P<0.00001); 4. UA: The decrease in CRRT group was higher than that in the internal medicine drug treatment group[MD=-95.05, 95%CI(-156.94, -33.16), P=0.003], (I²=80%, P=0.002); 5. BNP: The reduction effect of CRRT group is better than that of internal medicine drug treatment group[MD=-474.92, 95%CI(-636.76, -313.09), P<0.00001], (I²=91%,P<0.00001); 6. LVD: The CRRT group showed better reduction than the internal medicine drug treatment group[MD=-3.97, 95%CI(-6.75, -1.19), P=0.005], (I²=0%, P=0.002); 7. Urine output: The CRRT group showed better recovery than the internal medicine drug treatment group[MD=87.91, 95%CI(38.09, 137.73), P=0.0005], (I²=84%, P=0.002); 8. Classification of cardiac function: The downgrading effect of the CRRT group is better than that of the internal medicine drug treatment group[MD=-1.10, 95%CI(-1.43, -0.78), P<0.00001], (I²=76%, P=0.02); 9. GFR: The increase in CRRT group was better than that in the internal medicine drug treatment group[MD=21.36,95%CI(18.59, 24.13), P<0.00001], (I²=0%, P=0.73); 10.Ccr:The recovery of the CRRT group was better than that of the internal medicine drug treatment group[MD=7.68,95%CI(4.52, 10.83)P<0.00001](I²=82%, P=0.02); 11.SV: There was no statistically significant difference between the CRRT group and the internal medicine treatment group[MD=2.35, 95%CI(-3.38, 8.07), P=0.42], (I²=92%, P=0.0006); 12. CysC: There was no statistically significant difference between the CRRT group and the internal medicine treatment group[MD=-1.13, 95%CI(-2.41, 0.15), P=0.08], (I²=95%, P=0.00001); 13. K+: There was no statistically significant difference between the CRRT group and the internal medicine treatment group[MD=-0.15, 95%CI(-0.31, 0.01), P=0.07], (I²=0%, P=0.75).
References
[2] Kellum, J. A., Bellomo, R., & Ronco, C. (2008). Acute Dialysis Quality Initiative (ADQI): Methodology. International Journal of Artificial Organs, 31(2), 90–93. https://doi.org/10.1177/039139880803100201
[3] Gao, Y., Xiu, M., & Bian, Y. (2015). Clinical efficacy of continuous renal replacement therapy in elderly patients with cardiorenal syndrome. Journal of Difficult Diseases, 14(10), 1039–1042.
[4] Ronco, C., Bellasi, A., & Di Lullo, L. (2018). Cardiorenal syndrome: An overview. Advances in Chronic Kidney Disease, 25(5), 382–390. https://doi.org/10.1053/j.ackd.2018.08.004
[5] Liu, Y., & Qiu, G. (2016). Recombinant human brain natriuretic peptide combined with continuous renal replacement therapy for cardiorenal syndrome refractory heart failure observation. Chinese Pharmacists, 19(3), 532–534.
[6] Li, Y., Li, J., Niu, J., et al. (2017). Clinical experience of continuous renal replacement therapy in 20 cases of type II cardiorenal syndrome. Jilin Medical Journal, 38(2), 268–270.
[7] Acierno, M. J., & Maeckelbergh, V. (2008). Continuous renal replacement therapy. Compendium: Continuing Education for Veterinarians, 30(5), 264–272.
[8] Ding, H., Liu, D., & Zhou, X. (2011). Application of continuous renal replacement therapy in acute cardiorenal syndrome. Journal of Gerontology, 31(12), 2344–2345.
[9] Yu, Z., Liu, J., Li, X., et al. (2017). Clinical observation of continuous renal replacement therapy in refractory cardiorenal syndrome. Xinjiang Medical Journal, 47(7), 735–737.
[10] Shi, Y. (2023). Continuous renal replacement in the treatment of cardiorenal syndrome and severe heart failure in patients with clinical efficacy observation. Chinese Science and Technology Journal Database (Abstract Edition) Medical and Health, 2, 47–49.
[11] Song, Y., Liu, Y., Zhou, Q., et al. (2022). Effect of continuous renal replacement therapy in elderly patients with type 1 cardiorenal syndrome. Chinese and Foreign Medical Research, 20(27), 1–5.
[12] Yin, W., Xu, D., & Yang, J. (2014). Application analysis of continuous blood purification therapy in elderly patients with acute myocardial infarction complicated with cardiorenal syndrome. Chinese Medical Guideline, 12(5), 136–137.
[13] Xu, H., Huang, J., & Li, J. (2016). Clinical study of continuous renal replacement therapy for cardiorenal syndrome complicated with severe heart failure. Acta Academia Medicinae Qiqihar, 37(15), 1908–1909.
[14] Zhu, Y., Xu, H., & Zhou, W. (2014). Clinical study of continuous renal replacement therapy in the treatment of cardiorenal syndrome. Chinese Journal of Integrative Nephrology, 15(11), 991–992.
[15] Wu, Z., & Guo, Y. (2017). Clinical observation of continuous renal replacement therapy in the treatment of cardiorenal syndrome. Health Nutrition in China, 27(31), 84.
[16] Zhao, R. (2020). To explore the effect of continuous renal replacement therapy in the treatment of cardiorenal syndrome. Maternal World, 31, 64.
[17] Huo, F. (2012). Observation on the effect of continuous renal replacement therapy in the treatment of acute cardiorenal syndrome. Medicine, 18(36), 34–35.
[18] Damman, K., Tang, W. H. W., Testani, J. M., et al. (2014). Terminology and definition of changes renal function in heart failure. European Heart Journal, 35(48), 3413–3416. https://doi.org/10.1093/eurheartj/ehu320
[19] U.S. National Center for Health Statistics. (2018). Health, United States, 2017: With special feature on mortality. National Center for Health Statistics (US).
[20] Wang, X., & Cao, H. (2013). Research progress of acute cardiorenal syndrome. Medical Review, 19(7), 1265–1267.
[21] Yao, H., Wen, M., Huang, G., et al. (2011). Application of early high-flow continuous blood purification in severe acute pancreatitis. South China Journal of Defense Medicine, 25(3), 224–227.
[22] Heywood, J. T., Fonarow, G. C., Costanzo, M. R., et al. (2007). High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: A report from the ADHERE database. Journal of Cardiac Failure, 13(6), 422–430. https://doi.org/10.1016/j.cardfail.2007.03.011
[23] Takahama, H., & Kitakaze, M. (2017). Pathophysiology of cardiorenal syndrome in patients with heart failure: Potential therapeutic targets. American Journal of Physiology-Heart and Circulatory Physiology, 313(4), H715–H721. https://doi.org/10.1152/ajpheart.00215.2017
[24] Mavrakanas, T. A., Khattak, A., Singh, K., et al. (2017). Epidemiology and natural history of the cardiorenal syndromes in a cohort with echocardiography. Clinical Journal of the American Society of Nephrology, 12(10), 1624–1633. https://doi.org/10.2215/CJN.00670117
[25] De Castro, F. D., Chaves, P. C., & Leite-Moreira, A. F. (2010). Cardiorenal syndrome and its pathophysiological implications. Revista Portuguesa de Cardiologia, 29(10), 1535–1554.
[26] Zannad, F., & Rossignol, P. (2018). Cardiorenal syndrome revisited. Circulation, 138(9), 929–944. https://doi.org/10.1161/CIRCULATIONAHA.117.028814
[27] Cheng, W., & Zhang, Y. (2020). Cardiorenal syndrome. Journal of Cardiovascular Rehabilitation Medicine, 29(3), 396–399.
[28] Junho, C., Caio-Silva, W., Trentin-Sonoda, M., et al. (2020). An overview of the role of calcium/calmodulin-dependent protein kinase in cardiorenal syndrome. Frontiers in Physiology, 11, Article 735. https://doi.org/10.3389/fphys.2020.00735
[29] Li, J., Li, C., Li, L., et al. (2023). The pathogenesis, diagnosis and treatment progress of cardiorenal syndrome. Chinese Cardiovascular Disease Research, 21(6), 493–498.
[30] Felker, G. M., Lee, K. L., Bull, D. A., et al. (2011). Diuretic strategies in patients with acute decompensated heart failure. New England Journal of Medicine, 364(9), 797–805. https://doi.org/10.1056/NEJMoa1005419
[31] Cao, X., & Zhang, L. (2015). Rational application of diuretics in patients with heart failure. Electronic Journal of Integrative Cardiovascular Disease, 3(30), 1–4.
[32] Jain, A., Agrawal, N., & Kazory, A. (2016). Defining the role of ultrafiltration therapy in acute heart failure: A systematic review and meta-analysis. Heart Failure Reviews, 21(5), 611–619. https://doi.org/10.1007/s10741-016-9559-2
[33] Luo, Y., Li, L., Ye, X., et al. (2023). The therapeutic effect of diuretics combined with RAAS antagonists on cardiorenal syndrome. Chinese Medical Innovation, 20(19), 76–81.
[34] McDonagh, T. A., Metra, M., Adamo, M., et al. (2021). 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal, 42(36), 3599–3726. https://doi.org/10.1093/eurheartj/ehab368
[35] Weir, M. R., Lakkis, J. I., Jaar, B., et al. (2018). Use of renin-angiotensin system blockade in advanced CKD: An NKF-KDOQI controversies report. American Journal of Kidney Diseases, 72(6), 873–884. https://doi.org/10.1053/j.ajkd.2018.06.010
[36] Bai, X., Zhao, H., Kang, D., et al. (2021). Clinical effect observation of bedside blood purification combined with rhBNP in the treatment of cardiorenal syndrome. Journal of Clinical Military Medicine, 49(5), 562–563.
[37] He, Y. (2021). Effect of hemodialysis in the treatment of patients with nephrotic syndrome and acute renal failure. Chinese Medical Guideline, 19(12), 104–105.
[38] Xiong, J. (2020). To explore and analyze the mental health and clinical effect of hemodialysis ultrafiltration in patients with severe nephrotic edema. Smart Health, 6(34), 49–51.
[39] Fu, G. (2020). The treatment and effect of hemodialysis instrument in patients with acute renal failure of nephrotic syndrome. China Medical Device Information, 26(22), 35–36.
[40] Liang, J., Mai, J., Zeng, Z., et al. (2020). Comparison of clinical efficacy of different hemodialysis methods in the treatment of cardiorenal syndrome. Shenzhen Journal of Integrative Medicine, 30(20), 175–177.
[41] Badawy, S. S., & Fahmy, A. (2012). Efficacy and cardiovascular tolerability of continuous veno-venous hemodiafiltration in acute decompensated heart failure: A randomized comparative study. Journal of Critical Care, 27(1), 106–107. https://doi.org/10.1016/j.jcrc.2011.06.007
[42] Giglioli, C., Landi, D., Cecchi, E., et al. (2011). Effects of ultrafiltration vs. diuretics on clinical, biohumoral and haemodynamic variables in patients with decompensated heart failure: The ULTRADISCO study. European Journal of Heart Failure, 13(3), 337–346. https://doi.org/10.1093/eurjhf/hfq207

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)