Parkinson's Disease as a Risk Factor for Dental Caries? – Results of a Systematic Review
Abstract
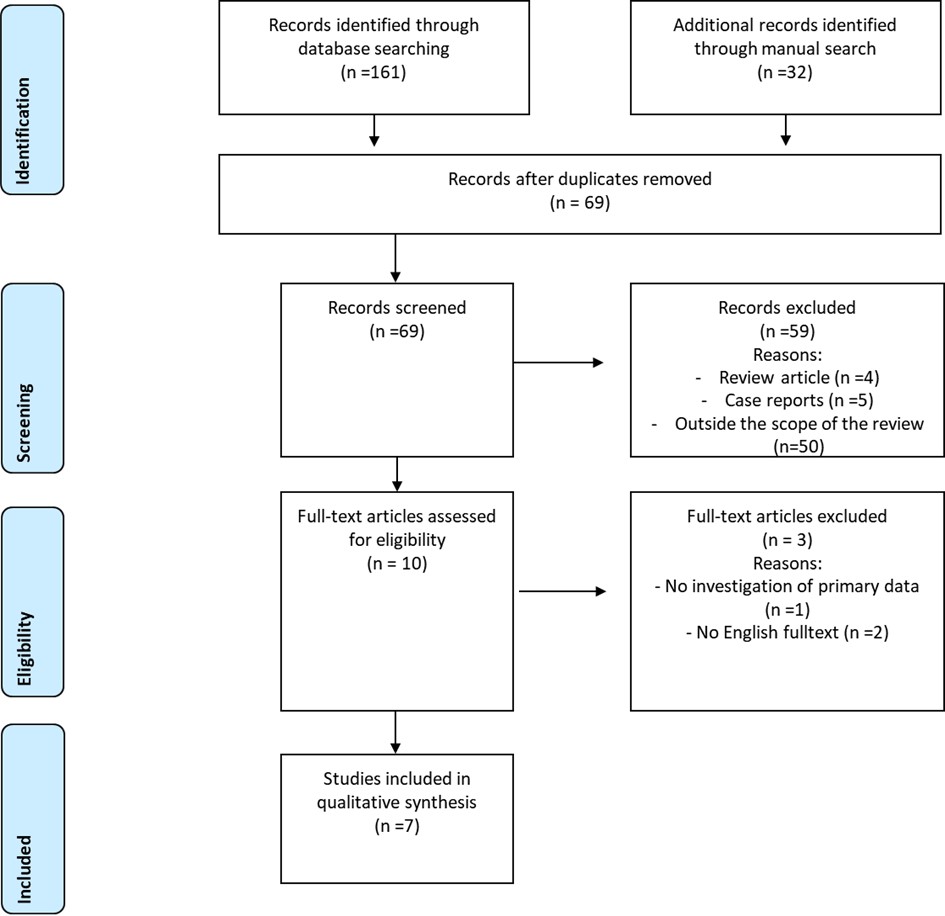
This systematic review aimed in the evaluation of dental caries in patients suffering from Parkinsons disease (PD), to answer the question, whether PD patients show a higher caries burden compared to controls. In January 2025, a systematic literature search in the platforms PubMed, Scopus and Web of Science was performed, using the search terms “parkinson” AND “caries” and “parkinson’s disease” AND “caries”. Data of studies, which also included a control group were extracted and qualitatively analyzed. The whole process was performed by two independent reviewers. Furthermore, a quality appraisal was performed. Overall, seven studies were included in the qualitative analysis, which originated from six different countries and included between 30 and 104 participants in the PD group. The de-ceased-, missing- and filled-teeth index (DMFT) was the most frequent caries assessment. In 5 of the 7 studies a significant difference in caries prevalence was found between patients with PD and controls, whereby only 3 of these studies showed worse caries burden in PD group. Moreover, it was shown that most of included studies were assessed to be of moderate quality. In conclusion, it can be stated that while the evidence for a higher caries prevalence of PD patients compared with controls is weak, burden of caries in patients with PD is high. Patients with PD should receive increased attention in dental care.
References
[2] Hirsch, L., Jette, N., Frolkis, A., Steeves, T., & Pringsheim, T. (2016). The incidence of Parkinson's disease: A systematic review and meta-analysis. Neuroepidemiology, 46(4), 292–300. https://doi.org/10.1159/000445751
[3] Pringsheim, T., Jette, N., Frolkis, A., & Steeves, T. D. (2014). The prevalence of Parkinson's disease: A systematic review and meta-analysis. Movement Disorders, 29(13), 1583–1590. https://doi.org/10.1002/mds.25945
[4] Siciliano, M., Trojano, L., Santangelo, G., De Micco, R., Tedeschi, G., & Tessitore, A. (2018). Fatigue in Parkinson's disease: A systematic review and meta-analysis. Movement Disorders, 33(11), 1712–1723. https://doi.org/10.1002/mds.27461
[5] Baiano, C., Barone, P., Trojano, L., & Santangelo, G. (2020). Prevalence and clinical aspects of mild cognitive impairment in Parkinson's disease: A meta-analysis. Movement Disorders, 35(1), 45–54. https://doi.org/10.1002/mds.27902
[6] Auffret, M., Meuric, V., Boyer, E., Bonnaure-Mallet, M., & Vérin, M. (2021). Oral health disorders in Parkinson's disease: More than meets the eye. Journal of Parkinson's Disease, 11(4), 1507–1535. https://doi.org/10.3233/JPD-212605
[7] Fleury, V., Zekeridou, A., Lazarevic, V., Gaïa, N., Giannopoulou, C., Genton, L., ... Burkhard, P. R. (2021). Oral dysbiosis and inflammation in Parkinson's disease. Journal of Parkinson's Disease, 11(2), 619–631. https://doi.org/10.3233/JPD-202459
[8] Silva, P. F., Biasotto-Gonzalez, D. A., Motta, L. J., Silva, S. M., Ferrari, R. A., Fernandes, K. P., & Bussadori, S. K. (2015). Impact in oral health and the prevalence of temporomandibular disorder in individuals with Parkinson's disease. Journal of Physical Therapy Science, 27(3), 887–891. https://doi.org/10.1589/jpts.27.887
[9] Verhoeff, M. C., Lobbezoo, F., van Leeuwen, A. M., Schuller, A. A., & Koutris, M. (2022). Oral health-related quality of life in patients with Parkinson's disease. Journal of Oral Rehabilitation, 49(4), 398–406. https://doi.org/10.1111/joor.13304
[10] Botelho, J., Machado, V., Mendes, J. J., & Mascarenhas, P. (2021). Causal association between periodontitis and Parkinson's disease: A bidirectional Mendelian randomization study. Genes, 12(5), 772. https://doi.org/10.3390/genes12050772
[11] Kaur, T., Uppoor, A., & Naik, D. (2016). Parkinson's disease and periodontitis – The missing link? A review. Gerodontology, 33(4), 434–438. https://doi.org/10.1111/ger.12188
[12] Peres, M. A., Macpherson, L. M. D., Weyant, R. J., Daly, B., Venturelli, R., Mathur, M. R., ... Watt, R. G. (2019). Oral diseases: A global public health challenge. The Lancet, 394(10194), 249–260. https://doi.org/10.1016/S0140-6736(19)31146-8
[13] Pitts, N. B., Zero, D. T., Marsh, P. D., Ekstrand, K., Weintraub, J. A., Ramos-Gomez, F., ... Ismail, A. (2017). Dental caries. Nature Reviews Disease Primers, 3, 17030. https://doi.org/10.1038/nrdp.2017.30
[14] Kutsch, V. K. (2014). Dental caries: An updated medical model of risk assessment. The Journal of Prosthetic Dentistry, 111(4), 280–285. https://doi.org/10.1016/j.prosdent.2013.07.014
[15] Hanaoka, A., & Kashihara, K. (2009). Increased frequencies of caries, periodontal disease and tooth loss in patients with Parkinson's disease. Journal of Clinical Neuroscience, 16(10), 1279–1282. https://doi.org/10.1016/j.jocn.2008.12.027
[16] Kreher, D., Ernst, B. L. V., Ziebolz, D., Haak, R., de Fallois, J., Ebert, T., & Schmalz, G. (2023). Prevalence of dental caries in patients on renal replacement therapy – A systematic review. Journal of Clinical Medicine, 12(4), 1507. https://doi.org/10.3390/jcm12041507
[17] Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097. https://doi.org/10.1371/journal.pmed.1000097
[18] Rostom, A., Dube, C., Cranney, A., et al. (2004). Celiac disease. Evidence Reports/Technology Assessments, No. 104. Agency for Healthcare Research and Quality (US). https://www.ncbi.nlm.nih.gov/books/NBK35156/
[19] Kieser, J., Jones, G., Borlase, G., & MacFadyen, E. (1999). Dental treatment of patients with neurodegenerative disease. New Zealand Dental Journal, 95(422), 130–134.
[20] de Baat, C., van Stiphout, M. A. E., & Lobbezoo, F. (2020). De objectieve mondgezondheid van personen met de ziekte van Parkinson [The objective oral health of Parkinson's disease patients]. Nederlands Tijdschrift voor Tandheelkunde, 127(5), 318–322. https://doi.org/10.5177/ntvt.2020.05.19131
[21] Maarel-Wierink, C. D. V., & Stiphout, M. A. E. V. (2021). Multifactoriële cariësprogressie bij Parkinson [Botox injections in salivary glands in Parkinson's disease]. Nederlands Tijdschrift voor Tandheelkunde, 128(10), 479–483. https://doi.org/10.5177/ntvt.2021.10.21081
[22] Müller, T., Palluch, R., & Jackowski, J. (2011). Caries and periodontal disease in patients with Parkinson's disease. Special Care in Dentistry, 31(5), 178–181. https://doi.org/10.1111/j.1754-4505.2011.00205.x
[23] Einarsdóttir, E. R., Gunnsteinsdóttir, H., Hallsdóttir, M. H., Sveinsson, S., Jónsdóttir, S. R., Olafsson, V. G., ... Holbrook, W. P. (2009). Dental health of patients with Parkinson's disease in Iceland. Special Care in Dentistry, 29(3), 123–127. https://doi.org/10.1111/j.1754-4505.2009.00075.x
[24] Fukayo, S., Nonaka, K., Shimizu, T., & Yano, E. (2003). Oral health of patients with Parkinson's disease: Factors related to their better dental status. Tohoku Journal of Experimental Medicine, 201(3), 171–179. https://doi.org/10.1620/tjem.201.171
[25] Persson, M., Osterberg, T., Granérus, A. K., & Karlsson, S. (1992). Influence of Parkinson's disease on oral health. Acta Odontologica Scandinavica, 50(1), 37–42. https://doi.org/10.3109/00016359209012744
[26] Cicciù, M., Risitano, G., Lo Giudice, G., & Bramanti, E. (2012). Periodontal health and caries prevalence evaluation in patients affected by Parkinson's disease. Parkinson’s Disease, 2012, 541908. https://doi.org/10.1155/2012/541908
[27] García-De-La-Fuente, A. M., Lafuente-Ibáñez-de-Mendoza, I., Lartitegui-Sebastián, M. J., Marichalar-Mendia, X., Echebarria-Goikouria, M. Á., & Aguirre-Urizar, J. M. (2022). Facts and controversies regarding oral health in Parkinson's disease: A case-control study in Spanish patients. Medicina Oral, Patología Oral y Cirugía Bucal, 27(5), e419–e425. https://doi.org/10.4317/medoral.25348
[28] López, R., Smith, P. C., Göstemeyer, G., & Schwendicke, F. (2017). Ageing, dental caries and periodontal diseases. Journal of Clinical Periodontology, 44(Suppl 18), S145–S152. https://doi.org/10.1111/jcpe.12683
[29] Thomson, W. M., Broadbent, J. M., Foster Page, L. A., & Poulton, R. (2013). Antecedents and associations of root surface caries experience among 38-year-olds. Caries Research, 47, 128–134. https://doi.org/10.1159/000345078
[30] Takano, N., Ando, Y., Yoshihara, A., & Miyazaki, H. (2003). Factors associated with root caries incidence in an elderly population. Community Dental Health, 20, 217–222.
[31] Phelan, J. A., Mulligan, R., Nelson, E., Brunelle, J., Alves, M. E., Navazesh, M., & Greenspan, D. (2004). Dental caries in HIV-seropositive women. Journal of Dental Research, 83, 869–873. https://doi.org/10.1177/154405910408301109
[32] Zlotnik, Y., Balash, Y., Korczyn, A. D., Giladi, N., & Gurevich, T. (2015). Disorders of the oral cavity in Parkinson's disease and parkinsonian syndromes. Parkinson’s Disease, 2015, 379482. https://doi.org/10.1155/2015/379482
[33] Schmalz, G., Garbade, J., Kollmar, O., & Ziebolz, D. (2020). Does oral health-related quality of life of patients after solid organ transplantation indicate a response shift? Results of a systematic review. BMC Oral Health, 20(1), 356. https://doi.org/10.1186/s12903-020-01350-w
[34] Schmalz, G., Denkler, C. R., Kottmann, T., Rinke, S., & Ziebolz, D. (2021). Oral health-related quality of life, oral conditions, and risk of malnutrition in older German people in need of care – A cross-sectional study. Journal of Clinical Medicine, 10(3), 426. https://doi.org/10.3390/jcm10030426
[35] Ouanounou, A. (2016). Xerostomia in the geriatric patient: Causes, oral manifestations, and treatment. Compendium of Continuing Education in Dentistry, 37(5), 306–311.
[36] Barbe, A. G. (2018). Medication-induced xerostomia and hyposalivation in the elderly: Culprits, complications, and management. Drugs & Aging, 35(10), 877–885. https://doi.org/10.1007/s40266-018-0588-5
[37] Machiulskiene, V., Campus, G., Carvalho, J. C., Dige, I., Ekstrand, K. R., Jablonski-Momeni, A., ... Nyvad, B. (2020). Terminology of dental caries and dental caries management: Consensus report of a workshop organized by ORCA and Cariology Research Group of IADR. Caries Research, 54(1), 7–14. https://doi.org/10.1159/000503309
[38] World Health Organization. (1997). Oral health surveys: Basic methods (4th ed.). WHO, Oral Health Unit.
[39] Kapor, S., Rankovic, M. J., Khazaei, Y., Crispin, A., Schüler, I., Krause, F., ... Kühnisch, J. (2021). Systematic review and meta-analysis of diagnostic methods for occlusal surface caries. Clinical Oral Investigations, 25(8), 4801–4815. https://doi.org/10.1007/s00784-021-04024-1
[40] Rankovic, M. J., Kapor, S., Khazaei, Y., Crispin, A., Schüler, I., et al. (2021). Systematic review and meta-analysis of diagnostic studies of proximal surface caries. Clinical Oral Investigations, 25(11), 6069–6079. https://doi.org/10.1007/s00784-021-04113-1
[41] AlQranei, M. S., Balhaddad, A. A., & Melo, M. A. S. (2021). The burden of root caries: Updated perspectives and advances on management strategies. Gerodontology, 38(2), 136–153. https://doi.org/10.1111/ger.12511
[42] Bignozzi, I., Crea, A., Capri, D., Littarru, C., Lajolo, C., & Tatakis, D. N. (2014). Root caries: A periodontal perspective. Journal of Periodontal Research, 49(2), 143–163. https://doi.org/10.1111/jre.12094

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)