The Relationship Between Educational Achievement and Oral Health Status: A Systematic Review of Cross-Sectional Studies
Abstract
Background: Oral health status significantly affects general health and quality of life, with mounting evidence suggesting a positive correlation between educational level and oral health outcomes. However, comprehensive synthesis of this relationship across diverse populations and healthcare systems remains limited.
Objective: To systematically review and analyze the relationship between educational level and oral health status across global populations, providing evidence-based insights for health policy development and oral health improvement strategies.
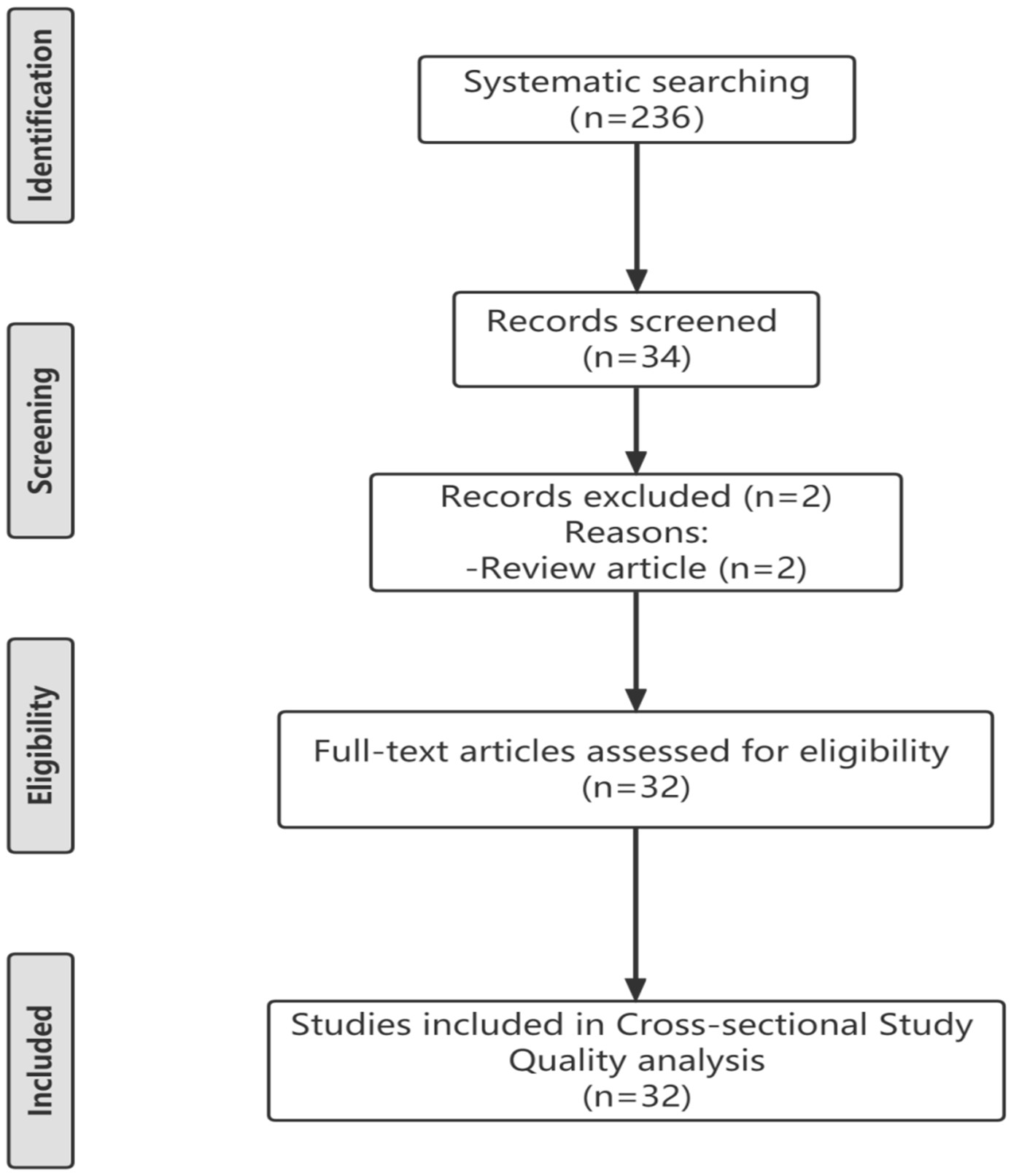
Methods: A systematic literature search was conducted using PubMed and The Cochrane Library databases from January 2007 to January 2025. Search terms included "oral health," "education level," "caries," "periodontosis," and "tooth loss." Cross-sectional studies examining the relationship between educational attainment and oral health outcomes were included. Study quality was assessed using the Agency for Healthcare Research and Quality 11-item checklist. Data extraction focused on correlations between educational level and dental caries, periodontal disease, and tooth loss across different populations and healthcare systems.
Results: A total of 236 articles were identified, with 32 cross-sectional studies meeting inclusion criteria after systematic screening. The studies encompassed populations from both developed countries (Britain, United States, Germany, Denmark, Belgium, Finland) and developing nations (Chile, Egypt, India, Thailand, Colombia, Nigeria, China). Consistent evidence demonstrated that educational level was negatively correlated with the prevalence of dental caries, periodontal disease, and tooth loss across all examined populations. This inverse relationship persisted even in developed countries with established national public health insurance systems, indicating that educational gradients in oral health transcend healthcare access barriers.
Conclusions: Educational level demonstrates a robust and consistent association with oral health outcomes across diverse global populations and healthcare systems. The universality of this relationship suggests that expanding educational opportunities represents a promising upstream intervention strategy for improving population oral health. These findings support the integration of educational advancement into comprehensive oral health promotion policies and highlight the potential for educational interventions to address oral health disparities at the population level.
References
[2] Petersen, P. E., Bourgeois, D., Ogawa, H., Estupinan-Day, S., & Ndiaye, C. (2005). The global burden of oral diseases and risks to oral health. Bulletin of the World Health Organization, 83, 661–669.
[3] Peres, M. A., Macpherson, L. M. D., Weyant, R. J., Daly, B., Venturelli, R., Mathur, M. R., ... & Watt, R. G. (2019). Oral diseases: A global public health challenge. The Lancet, 394(10194), 249–260. https://doi.org/10.1016/S0140-6736(19)31146-8
[4] Ben-Shlomo, Y., & Kuh, D. (2002). A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. Oxford University Press, 285–293. https://doi.org/10.1093/ije/31.2.285
[5] Hybels, C. F., Wu, B., Landerman, L. R., Liang, J., & Bennett, J. M. (2016). Trends in decayed teeth among middle-aged and older adults in the United States: Socioeconomic disparities persist over time. Journal of Public Health Dentistry, 76(4), 287–294. https://doi.org/10.1111/jphd.12153
[6] Geyer, S., Schneller, T., & Micheelis, W. (2010). Social gradients and cumulative effects of income and education on dental health in the Fourth German Oral Health Study. Community Dentistry and Oral Epidemiology, 38(2), 120–128. https://doi.org/10.1111/j.1600-0528.2009.00520.x
[7] Bernabé, E., Suominen-Taipale, L., Nordblad, A., Savolainen, J., & Knuuttila, M. (2011). Education level and oral health in Finnish adults: Evidence from different lifecourse models. Journal of Clinical Periodontology, 38(1), 25–32. https://doi.org/10.1111/j.1600-051X.2010.01647.x
[8] Lambert, M., Keukeleire, L. D., Vandenbosch, K., Vanobbergen, J., & Hoppenbrouwers, K. (2018). Social gradient in caries experience of Belgian adults 2010. Community Dental Health, 35(3), 160–166.
[9] He, S., & Thomson, W. M. (2018). An oral epidemiological comparison of Chinese and New Zealand adults in 2 key age groups. Community Dentistry and Oral Epidemiology, 46(2), 154–160. https://doi.org/10.1111/cdoe.12348
[10] Guan, L., Li, X., Jin, H., Liu, Z., & Wang, B. (2020). Status of dental caries and associated factors in Tibetan adults: Findings from the Fourth China National Oral Health Survey. BMC Oral Health, 20(1), 248. https://doi.org/10.1186/s12903-020-01225-0
[11] Hessari, H., Vehkalahti, M. M., Eghbal, M. J., Murtomaa, H., & Vehkalahti, M. (2007). Oral health among 35- to 44-year-old Iranians. Medical Principles and Practice, 16(4), 280–285. https://doi.org/10.1159/000102150
[12] Borgeat Meza, M., Frenz, P., Araya, R., & Margozzini, P. (2022). Changes in oral health inequalities in adults in Chile. Community Dentistry and Oral Epidemiology, 50(6), 506–512. https://doi.org/10.1111/cdoe.12701
[13] Guarnizo-Herreño, C. C., Watt, R. G., Paredes-Dominguez, P., Garcia, J. L., & Marmot, M. G. (2019). Health insurance and education: Major contributors to oral health inequalities in Colombia. Journal of Epidemiology and Community Health, 73(8), 737–744. https://doi.org/10.1136/jech-2018-212049
[14] Bogale, B., Deyessa, N., & Wondimagegn, D. (2021). Dental caries experience and associated factors in adults: A cross-sectional community survey within Ethiopia. BMC Public Health, 21(1), 180. https://doi.org/10.1186/s12889-021-10199-9
[15] Tafere, Y., Chanie, S., & Dessie, G. (2018). Assessment of prevalence of dental caries and the associated factors among patients attending dental clinic in Debre Tabor General Hospital: A hospital-based cross-sectional study. BMC Oral Health, 18(1), 119. https://doi.org/10.1186/s12903-018-0581-8
[16] Baehni, P. C. (2012). Translating science into action—Prevention of periodontal disease at patient level. Periodontology 2000, 60(1), 162–172. https://doi.org/10.1111/j.1600-0757.2011.00428.x
[17] Baumeister, S. E., Kocher, T., & Holtfreter, B. (2022). Understanding the consequences of educational inequalities on periodontitis: A Mendelian randomization study. Journal of Clinical Periodontology, 49(3), 200–209. https://doi.org/10.1111/jcpe.13581
[18] Hakeem, F. F., & Sabbah, W. (2019). Is there socioeconomic inequality in periodontal disease among adults with optimal behaviours? Acta Odontologica Scandinavica, 77(5), 400–407. https://doi.org/10.1080/00016357.2019.1582795
[19] Schmidt, J. C., Schimmel, M., Schimmel, J., et al. (2020). Dental and periodontal health in a Swiss population-based sample of older adults: A cross-sectional study. European Journal of Oral Sciences, 128(6), 508–517. https://doi.org/10.1111/eos.12738
[20] Zhao, Q., Zhang, J., Sun, L., et al. (2019). Periodontal health: A national cross-sectional study of knowledge, attitudes and practices for the public oral health strategy in China. Journal of Clinical Periodontology, 46(4), 406–419. https://doi.org/10.1111/jcpe.13082
[21] Abou El Fadl, R. K., Hammad, S. M., El-Gendy, R. A., & Yousry, M. M. (2021). Periodontal diseases and potential risk factors in Egyptian adult population—Results from a national cross-sectional study. PLoS One, 16(11), e0258958. https://doi.org/10.1371/journal.pone.0258958
[22] Kassebaum, N. J., Smith, A. G. C., Bernabé, E., et al. (2014). Global burden of severe tooth loss: A systematic review and meta-analysis. Journal of Dental Research, 93(7 Suppl), 20s–28s. https://doi.org/10.1177/0022034514537828
[23] Tsakos, G., Watt, R. G., Rouxel, P., de Oliveira, C., & Demakakos, P. (2015). Tooth loss associated with physical and cognitive decline in older adults. Journal of the American Geriatrics Society, 63(1), 91–99. https://doi.org/10.1111/jgs.13190
[24] Sato, Y., Aida, J., Tsuboya, T., et al. (2016). Tooth loss and decline in functional capacity: A prospective cohort study from the Japan Gerontological Evaluation Study. Journal of the American Geriatrics Society, 64(11), 2336–2342. https://doi.org/10.1111/jgs.14324
[25] Aida, J., Kondo, K., Yamamoto, T., et al. (2011). Oral health and cancer, cardiovascular, and respiratory mortality of Japanese. Journal of Dental Research, 90(9), 1129–1135. https://doi.org/10.1177/0022034511414423
[26] Polzer, I., Schimmel, M., Müller, F., & Biffar, R. (2012). The association of tooth loss with all-cause and circulatory mortality. Is there a benefit of replaced teeth? A systematic review and meta-analysis. Clinical Oral Investigations, 16(2), 333–351. https://doi.org/10.1007/s00784-011-0625-9
[27] Matsuyama, Y., Jürges, H., & Listl, S. (2019). The causal effect of education on tooth loss: Evidence from United Kingdom schooling reforms. American Journal of Epidemiology, 188(1), 87–95. https://doi.org/10.1093/aje/kwy205
[28] Boillot, A., Peres, K. G., Peres, M. A., et al. (2018). Association between individual and neighbourhood socioeconomic factors and masticatory efficiency: A cross-sectional analysis of the Paris Prospective Study 3. Journal of Epidemiology and Community Health, 72(2), 132–139. https://doi.org/10.1136/jech-2017-209593
[29] Duijster, D., van Loveren, C., Dusseldorp, E., & Verrips, G. H. W. (2018). Material, behavioural, cultural and psychosocial factors in the explanation of socioeconomic inequalities in oral health. European Journal of Public Health, 28(4), 590–597. https://doi.org/10.1093/eurpub/ckx209
[30] Bachkati, K. H., Holm-Pedersen, P., Avlund, K., et al. (2017). Midlife cognitive ability, education, and tooth loss in older Danes. Journal of the American Geriatrics Society, 65(1), 194–199. https://doi.org/10.1111/jgs.14513
[31] Ishikawa, S., Nakamura, K., Kurioka, A., et al. (2019). Risk factors for tooth loss in community-dwelling Japanese aged 40 years and older: The Yamagata (Takahata) study. Clinical Oral Investigations, 23(4), 1753–1760. https://doi.org/10.1007/s00784-018-2604-x
[32] Koyama, S., Aida, J., Saito, M., et al. (2016). Community social capital and tooth loss in Japanese older people: A longitudinal cohort study. BMJ Open, 6(4), e010768. https://doi.org/10.1136/bmjopen-2015-010768
[33] Ando, A., Nagao, K., Tamaki, Y., et al. (2013). Factors related to tooth loss among community-dwelling middle-aged and elderly Japanese men. Journal of Epidemiology, 23(4), 301–306. https://doi.org/10.2188/jea.JE20120180
[34] Kim, Y. H., Lee, J. H., Kim, Y. H., & Choi, Y. H. (2018). Number of remaining teeth and its association with socioeconomic status in South Korean adults: Data from the Korean National Health and Nutrition Examination Survey 2012–2013. PLoS One, 13(5), e0196594. https://doi.org/10.1371/journal.pone.0196594
[35] Yu, N. H., Lee, J. H., Cho, K. H., et al. (2021). Estimation and change of edentulism among the Korean population: Korea National Health and Nutrition Examination Survey 2007–2018. Epidemiology and Health, 43, e2021020. https://doi.org/10.4178/epih.e2021020
[36] Li, S., Guo, Y., & Miao Jonasson, J. (2022). Association between social capital and oral health among adults aged 50 years and over in China: A cross-sectional study. BMC Oral Health, 22(1), 68. https://doi.org/10.1186/s12903-022-02102-8
[37] Ferreira, R. C., Martins, A. M. E. B. L., & Ferreira, E. F. E. (2020). Education and income-based inequality in tooth loss among Brazilian adults: Does the place you live make a difference? BMC Oral Health, 20(1), 246. https://doi.org/10.1186/s12903-020-01238-9
[38] Chalub, L. L., Martins, M. T., Ferreira, R. C., et al. (2016). Functional dentition in Brazilian adults: An investigation of social determinants of health (SDH) using a multilevel approach. PLoS One, 11(2), e0148859. https://doi.org/10.1371/journal.pone.0148859
[39] Vettore, M. V., et al. (2020). Individual- and city-level socioeconomic factors and tooth loss among elderly people: A cross-level multilevel analysis. International Journal of Environmental Research and Public Health, 17(7). https://doi.org/10.3390/ijerph17072345
[40] Margozzini, P., et al. (2020). Number of remaining teeth and its association with educational level in Chilean adults: Data from the National Health Survey 2016–2017. International Journal of Dentistry, 2020, 8848190. https://doi.org/10.1155/2020/8848190
[41] Ibiyemi, O., & Idiga, E. (2017). Tooth loss among the elders in an inner city area of Ibadan, Nigeria. Gerodontology, 34(2), 264–271. https://doi.org/10.1111/ger.12263
[42] Srisilapanan, P., Korwanich, N., & Lalloo, R. (2016). Associations between social inequality and tooth loss in a household sample of elderly Thai people aged ≥60 years old. Gerodontology, 33(2), 201–208. https://doi.org/10.1111/ger.12140
[43] Drewnowski, A., & Specter, S. E. (2004). Poverty and obesity: The role of energy density and energy costs. American Journal of Clinical Nutrition, 79(1), 6–16. https://doi.org/10.1093/ajcn/79.1.6
[44] Bordin, D., Fadel, C. B., & Silva, A. M. R. (2017). Determinants of oral self-care in the Brazilian adult population: A national cross-sectional study. Brazilian Oral Research, 31, e115. https://doi.org/10.1590/1807-3107bor-2017.vol31.0115
[45] Šiljak, S., et al. (2019). Dental service utilisation among adults in a European developing country: Findings from a national health survey. International Dental Journal, 69(3), 200–206. https://doi.org/10.1111/idj.12449
[46] Nyamuryekung'e, K. K., Lahti, S. M., & Tuominen, R. J. (2018). Attitudes towards tooth fillings in Tanzanian adults and its association with previous filling experience. BMC Oral Health, 18(1), 12. https://doi.org/10.1186/s12903-018-0474-x
[47] Vano, M., Gherlone, E., Gallusi, G., et al. (2015). The influence of educational level and oral hygiene behaviours on DMFT index and CPITN index in an adult Italian population: An epidemiological study. International Journal of Dental Hygiene, 13(2), 151–157. https://doi.org/10.1111/idh.12098
[48] Thompson, F. E., McNeel, T. S., Dowling, E. C., et al. (2009). Interrelationships of added sugars intake, socioeconomic status, and race/ethnicity in adults in the United States: National Health Interview Survey, 2005. Journal of the American Dietetic Association, 109(8), 1376–1383. https://doi.org/10.1016/j.jada.2009.05.002
[49] Gilman, S. E., Martin, L. T., Abrams, D. B., et al. (2008). Educational attainment and cigarette smoking: A causal association? International Journal of Epidemiology, 37(3), 615–624. https://doi.org/10.1093/ije/dym250
[50] Siukosaari, P., Ainamo, A., & Närhi, T. O. (2005). Level of education and incidence of caries in the elderly: A 5-year follow-up study. Gerodontology, 22(3), 130–136. https://doi.org/10.1111/j.1741-2358.2005.00070.x
[51] Grossman, M. (2022). The demand for health turns 50: Reflections. Health Economics, 31(9), 1807–1822. https://doi.org/10.1002/hec.4563

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)