Medication error in the provision of healthcare services
A Serious Public Health Concern
Abstract
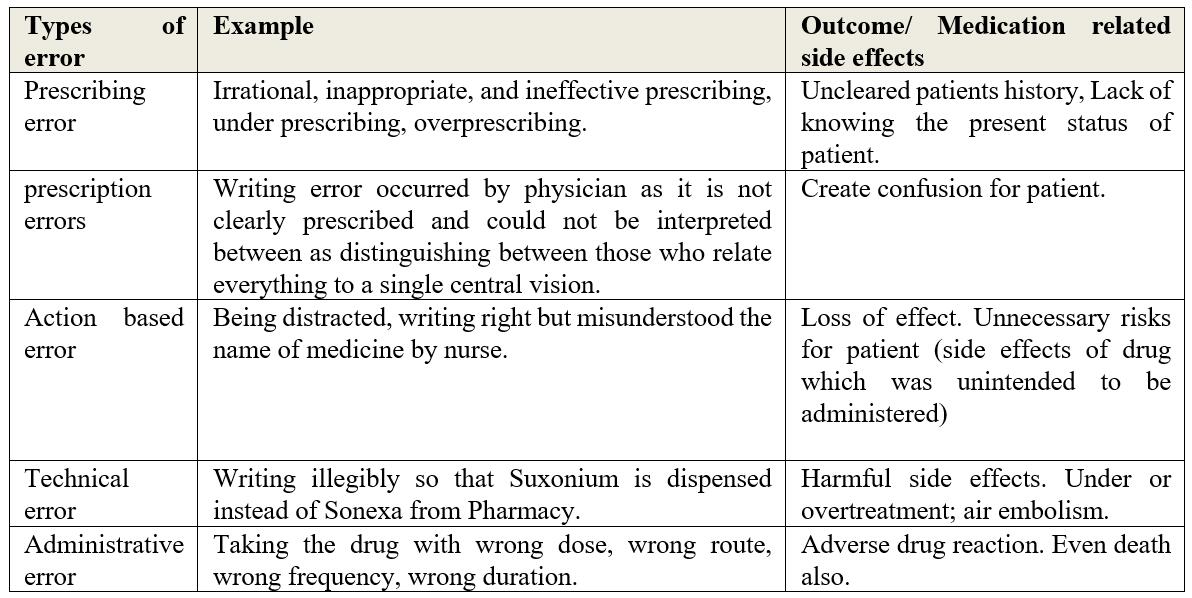
Medication errors are the most common and widespread medical adverse event that occurs in healthcare settings and can lead to increased patient morbidity, mortality, and healthcare costs. The availability of a wide range of over-the-counter and prescribed medications in the healthcare market, which the general public seems to use on a frequent basis to treat their health complications, has rapidly increased the chances of medication errors. Furthermore, the medication chain has several steps that require different people, and errors can occur at different stages in patient care, from ordering the medication to the time the patient is administered the drug. So each stage of the medication chain is exposed to risks that could result in medication errors. Thereby, medication errors prompt patient harm, preclude immediate discharges, and enhance healthcare costs. As a result, it is important to set up a medication safety culture that can light up in the context of effectively putting strategies into action, and everyone's collaboration and participation to adhering to medication safety strategy can improve patient safety. This review of the literature aims to provide a concept of medication errors, explore the pattern of errors, causes and consequences of errors, and error-related adverse events in all types of healthcare settings, risk factors for medication errors, and strategies to avoid and minimize medication errors.
References
[2] Medication error definition. Nccmerp.org. Retrieved from https://www.nccmerp.org/about-medication-errors
[3] Dean, B., Barber, N., & Schachter, M. (2000). What is a prescribing error? Qual Health Care.2000;9:232-7. Qual Health Care, 9, 232-237.
[4] Technical series on safer primary care medication errors: Technical series on safer primary care. Who.int. Retrieved from https://apps.who.int/iris/rest/bitstreams/1070139/retrieve
[5] Rasool, M. F., Rehman, A. ur, Imran, I., Abbas, S., Shah, S., Abbas, G., Khan, I., Shakeel, S., Ahmad Hassali, M. A., & Hayat, K. (2020). Risk factors associated with medication errors among patients suffering from chronic disorders. Frontiers in Public Health, 8. https://doi.org/10.3389/fpubh.2020.531038
[6] Kovačević, M., Vezmar Kovačević, S., Miljković, B., Radovanović, S., & Stevanović, P. (2017). The prevalence and preventability of potentially relevant drug-drug interactions in patients admitted for cardiovascular diseases: A cross-sectional study. International Journal of Clinical Practice, 71(10), e13005. https://doi.org/10.1111/ijcp.13005
[7] Fialová, D., Kummer, I., Držaić, M., & Leppee, M. (2018). Ageism in medication use in older patients. In International Perspectives on Aging (pp. 213-240). Springer International Publishing.
[8] Leone, R., Magro, L., Moretti, U., Cutroneo, P., Moschini, M., Motola, D., Tuccori, M., & Conforti, A. (2010). Identifying adverse drug reactions associated with drug-drug interactions: Data mining of a spontaneous reporting database in Italy. Drug Safety: An International Journal of Medical Toxicology and Drug Experience, 33(8), 667-675. https://doi.org/10.2165/11534400-000000000-00000
[9] Avery, A. A., Barber, N., Ghaleb, M., Franklin, D., & Crowe, A. S. (2012). Investigating the Prevalence and Causes of Prescribing Errors in General Practice: the Practice Study. General Medical Council.
[10] Claesson, C. B., Burman, K., Nilsson, J. L. G., & Vinge, E. (2011). Prescription errors detected by Swedish pharmacists. The International Journal of Pharmacy Practice, 3(3), 151-156. https://doi.org/10.1111/j.2042-7174.1995.tb00809.x
[11] Khoja, T., Neyaz, Y., Qureshi, N. A., Magzoub, M. A., Haycox, A., & Walley, T. (2011). Medication errors in primary care in Riyadh City, Saudi Arabia. La Revue de Sante de La Mediterranee Orientale [Eastern Mediterranean Health Journal], 17(2), 156-159. https://doi.org/10.26719/2011.17.2.156
[12] Zavaleta-Bustos, M., Castro-Pastrana, L. I., Reyes-Hernández, I., López-Luna, M. A., & Bermúdez-Camps, I. B. (2008). Prescription errors in a primary care university unit: urgency of pharmaceutical care in Mexico. Revista Brasileira de Ci?Ncias Farmac? Uticas, 44(1), 115-125. https://doi.org/10.1590/s1516-93322008000100013
[13] Masotti, P., McColl, M. A., & Green, M. (2010). Adverse events experienced by homecare patients: a scoping review of the literature. International Journal for Quality in Health Care, 22(2), 115-125. https://doi.org/10.1093/intqhc/mzq003
[14] Medication errors statistics 2023. (2021, May 2). The Checkup. Retrieved from https://www.singlecare.com/blog/news/medication-errors-statistics/
[15] Tariq, R. A., Vashisht, R., Sinha, A., & Scherbak, Y. (2023). Medication dispensing errors and prevention. StatPearls Publishing.
[16] Larrea Urtaran, X., Pérez Plasencia, A., Coma Punset, M., Dordà Benito, A., Ortí Juan, C., Nogue Pujadas, E., López Noguera, Q., Gratacos Santanach, L., Subirana Batlle, C., & Sacrest Güell, R. (2022). 5PSQ-104 Voluntary electronic reporting of medication errors and adverse drugs events during the first year of the COVID-19 pandemic. Section 5: Patient Safety and Quality Assurance.
[17] Alsulami, Z., Conroy, S., & Choonara, I. (2013). Medication errors in the Middle East countries: A systematic review of the literature. European Journal of Clinical Pharmacology, 69(4), 995-1008. https://doi.org/10.1007/s00228-012-1435-y
[18] Safety in Doses: Improving the Use of Medicines in the NHS. London: NPSA (2006). National Patient Safety Agency. The Report from the Patient Safety Observatory.
[19] Marjadi, B., & McLaws, M. L. (2010). Rural Indonesian health care workers’ constructs of infection prevention and control knowledge. American Journal of Infection Control, 38(5), 399-403. https://doi.org/10.1016/j.ajic.2009.11.010
[20] Navoa-Ng, J. A., Berba, R., Galapia, Y. A., Rosenthal, V. D., Villanueva, V. D., Tolentino, M. C. V., Genuino, G. A. S., Consunji, R. J., & Mantaring, J. B. V., 3rd. (2011). Device-associated infections rates in adult, pediatric, and neonatal intensive care units of hospitals in the Philippines: International Nosocomial Infection Control Consortium (INICC) findings. American Journal of Infection Control, 39(7), 548–554. https://doi.org/10.1016/j.ajic.2010.10.018
[21] Ernawati, D., Lee, Y. P., & Hughes, J. (2014). Nature and frequency of medication errors in a geriatric ward: an Indonesian experience. Therapeutics and Clinical Risk Management, 413. https://doi.org/10.2147/tcrm.s61687
[22] Nguyen, H.-T., Nguyen, T.-D., Haaijer-Ruskamp, F. M., & Taxis, K. (2014). Errors in preparation and administration of insulin in two urban Vietnamese hospitals: an observational study: An observational study. Nursing Research, 63(1), 68–72. https://doi.org/10.1097/NNR.0000000000000010
[23] Thu, T. A., Rahman, M., Coffin, S., Harun-Or-Rashid, M., Sakamoto, J., & Hung, N. V. (2012). Antibiotic use in Vietnamese hospitals: a multicenter point-prevalence study. American Journal of Infection Control, 40(9), 840–844. https://doi.org/10.1016/j.ajic.2011.10.020
[24] Cohen, M. R. (2023). Medication errors. Nursing, 53(9), 64. https://doi.org/10.1097/01.NURSE.0000946872.45300.63
[25] Aronson, J. K. (2009). Medication errors: what they are, how they happen, and how to avoid them. QJM: Monthly Journal of the Association of Physicians, 102(8), 513–521. https://doi.org/10.1093/qjmed/hcp052
[26] Jessurun, J. G., Hunfeld, N. G. M., de Roo, M., van Onzenoort, H. A. W., van Rosmalen, J., van Dijk, M., & van den Bemt, P. M. L. A. (2023). Prevalence and determinants of medication administration errors in clinical wards: A two‐centre prospective observational study. Journal of Clinical Nursing, 32(1-2), 208-220. https://doi.org/10.1111/jocn.16215
[27] Medication mistakes can have serious consequences. (2022, April 13). Raynes & Lawn Trial Lawyers. https://rayneslaw.com/medication-mistakes-can-have-serious-consequences/
[28] Hughes, R. G., & Ortiz, E. (2005). Medication errors: why they happen, and how they can be prevented. Journal of Infusion Nursing: The Official Publication of the Infusion Nurses Society, 28(2 Suppl), 14–24. https://doi.org/10.1097/00129804-200503001-00005
[29] American society of hospital pharmacists. ASHP guidelines for preventing medication errors in hospitals. (1993). Am J Hosp Pharm, 50, 305-314.
[30] Rogers, E., Griffin, E., Carnie, W., Melucci, J., & Weber, R. J. (2017). A Just Culture approach to managing medication errors. Hospital Pharmacy, 52(4), 308-315. https://doi.org/10.1310/hpj5204-308
[31] Mulac, A., Taxis, K., Hagesaether, E., & Gerd Granas, A. (2021). Severe and fatal medication errors in hospitals: findings from the Norwegian Incident Reporting System. European Journal of Hospital Pharmacy. Science and Practice, 28(e1), e56–e61. https://doi.org/10.1136/ejhpharm-2020-002298
[32] Gladstein, S. (2019, September 22). Consequences of medication errors - gladstein law firm, PLLC. Gladstein Law Firm; Gladstein Law Firm, PLLC. https://gladsteinlawfirm.com/blog/what-are-the-consequences-of-medication-errors/
[33] Morelock, S. (2016, August 2). Factors influencing nurse medication errors. RN Journal. https://rn-journal.com/journal-of-nursing/factors-influencing-nurse-medication-errors
[34] Michalek, C., Paparella, S., & Mandrack, M. (2022) High-alert medications heparin, concentrated electrolytes and magnesium: Practical strategies in pursuit of safety. Ismp.org. Retrieved from https://www.ismp.org/sites/default/files/attachments/2022-01/Baxter%20High%20Alert%20Part%202%20handouts.pdf
[35] Rankin, A., Cadogan, C. A., Patterson, S. M., Kerse, N., Cardwell, C. R., Bradley, M. C., Ryan, C., & Hughes, C. (2018). Interventions to improve the appropriate use of polypharmacy for older people. The Cochrane Library, 2018(9). https://doi.org/10.1002/14651858.cd008165.pub4
[36] Tek, S., & Topuz, A. (n.d.). The effect of the health literacy levels of parents on medication errors. Internationaljournalofcaringsciences.org. Retrieved December 27, 2023, from http://www.internationaljournalofcaringsciences.org/docs/64_tek_original_14-2.pdf
[37] Promoting rational use of medicines. WHO.int. Retrieved from http://www.who.int/medicines/areas/rational_use/en/
[38] Efstratios, A. (2014). An inside look into the factors contributing to medication errors in the clinical nursing practice. ICUS and Nursing Web Journal, 8(1), 0-0. Retrieved from https://www.itmedicalteam.pl/articles/an-inside-look-into-the-factors-contributing-to-medication-errors-in-the-clinical-nursing-practice-105510.html
[39] Damin Abukhalil, A., Amer, N. M., Musallam, L. Y., & Al-Shami, N. (2022). Medication error awareness among health care providers in Palestine: A questionnaire-based cross-sectional observational study. Saudi Pharmaceutical Journal: SPJ: The Official Publication of the Saudi Pharmaceutical Society, 30(4), 470-477. https://doi.org/10.1016/j.jsps.2022.01.014
[40] Moyen, E., Camiré, E., & Stelfox, H. (2008). Clinical review: Medication errors in critical care. Critical Care (London, England), 12(2), 208. https://doi.org/10.1186/cc6813
[41] Saljoughian, M., & PhD Department of Pharmacy Alta Bates Summit Medical Center Berkeley. (2020, June 18). Avoiding medication errors. Uspharmacist.com. Retrieved from https://www.uspharmacist.com/article/avoiding-medication-errors

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)