Issues Which Marginalize Females with ADHD - A Mixed Methods Systematic Review
Abstract
Background
Marked disadvantages of females with ADHD were identified by previous narrative reviews. Factors side-lining females with ADHD appear to be both biological and sociological in nature. Some published systematic reviews have focused on circumscribed aspects of female ADHD. An all-inclusive systematic review of the inequities which confer a status of marginalization to females with ADHD is required, to comprehensively understand all implications of female ADHD.
Objectives
The aim of this review was to identify and synthesize quantitative and qualitative evidence of issues which marginalize females with ADHD.
Methods
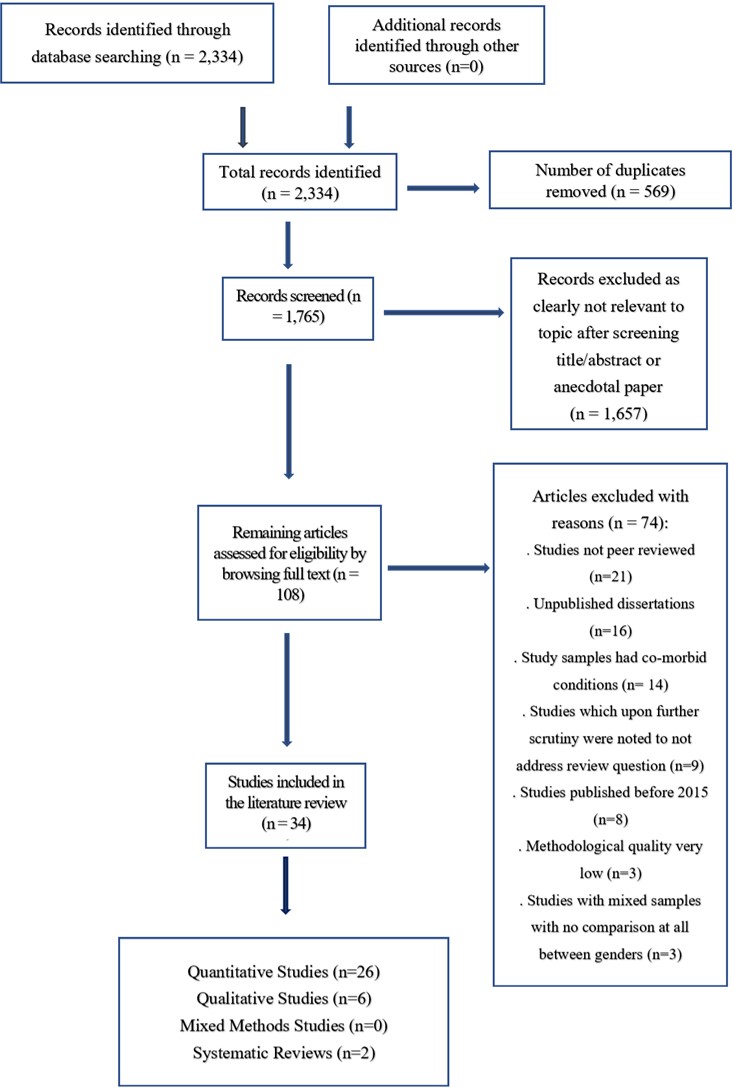
A mixed methods systematic review following a convergent integrated approach, as outlined by the Joanna Briggs Institute’s manual for evidence synthesis was undertaken. Databases were accessed through the Hydro Data Initiative platform of the University of Malta. All types of studies were considered for inclusion. Extracted quantitative findings were transformed into qualitative findings prior to synthesis. The review protocol was registered with PROSPERO CRD42022384055.
Results
34 papers were included in the review. Synthesis led to the emergence of five themes, namely ‘The gender gap in ADHD recognition, diagnosis and treatment’, ‘ADHD-related problems in females’, ‘Female ADHD and negative mental health sequelae’, ‘ADHD and female sexual and reproductive health issues’ and ‘The influence of ADHD on motherhood’.
Conclusions
Critically appraised, synthesized findings conclude that females with ADHD are disadvantaged in a number of ways. Clinicians and policy makers have access to latest evidence on all issues marginalizing females with ADHD in this mixed methods systematic review. Recommendations for policy and practice are advanced, together with directions future research ought to follow.
References
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). American Psychiatric Publishing, Inc..
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Attoe, D. E., & Climie, E. A. (2023). Miss. Diagnosis: A Systematic Review of ADHD in Adult Women. Journal of Attention Disorders, 27(7), 645-657. https://doi-org.ejournals.um.edu.mt/10.1177/10870547231161533
Babinski, D. E., Neely, K. A., Ba, D. M., & Liu, G. (2020). Depression and suicidal behavior in young adult men and women with ADHD: Evidence from claims data. The Journal of clinical psychiatry, 81(6), 22578. https://doi.org/10.4088/JCP.19m13130
Babinski, D., Shroff, D. M., Cao, V. T., & Waschbusch, D. A. (2021). Sex-Specific Norms for Diagnosing Attention-Deficit/Hyperactivity Disorder in Childhood: A Receiver Operating Characteristic (ROC) Analysis. Evidence-Based Practice in Child and Adolescent Mental Health, 6(2), 290-301. https://doi.org/10.1080/23794925.2021.1875343
Barentsen, R., van de Weijer, P. H., van Gend, S., & Foekema, H. (2001). Climacteric symptoms in a representative Dutch population sample as measured with the Greene Climacteric Scale. Maturitas, 38(2), 123-128. https://doi.org/10.1016/S0378-5122(00)00212-7
Beheshti, A., Chavanon, M. L., Schneider, S., & Christiansen, H. (2021). ADHD overdiagnosis and the role of patient gender among Iranian psychiatrists. BMC psychiatry, 21(1), 1-13. https://doi.org/10.1186/s12888-021-03525-3
Camara, B., Padoin, C., & Bolea, B. (2021). Relationship between sex hormones, reproductive stages and ADHD: a systematic review. Archives of women's mental health, 1-8. https://doi-org.ejournals.um.edu.mt/10.1177/10870547231161533
Dang, D., Dearholt, S. L., Bissett, K., Ascenzi, J., & Whalen, M. (2021). Johns Hopkins evidence-based practice for nurses and healthcare professionals: Model and guidelines. Sigma Theta Tau. https://apn.mhmedical.com/book.aspx?bookid=3144#264685080
Dorani, F., Bijlenga, D., Beekman, A. T., van Someren, E. J., & Kooij, J. S. (2021). Prevalence of hormone-related mood disorder symptoms in women with ADHD. Journal of psychiatric research, 133, 10-15. https://doi.org/10.1016/j.jpsychires.2020.12.005
Ersoy, M. A., & Topçu Ersoy, H. (2019). Gender-role attitudes mediate the effects of adult ADHD on marriage and relationships. Journal of attention disorders, 23(1), 40-50. https://doi.org/10.1177/1087054715618789
Eryılmaz, E., & Üstündağ-Budak, A. M. (2019). Gender bias in early recognition of ADHD. Turk Psikoloji Yazilari, 22(43), 102-104. https://doi.org/10.31828/tpy1301996120180710m000007
Evans-Agnew, R. A., & Strack, R. W. (2022). Photovoice: the little method that could change the world. Health Promotion Practice, 23(2), 201-204. https://doi.org/10.1177/15248399211069151
Fuller‐Thomson, E., Lewis, D. A., & Agbeyaka, S. K. (2016). Attention‐deficit/hyperactivity disorder casts a long shadow: findings from a population‐based study of adult women with self‐reported ADHD. Child: Care, Health and Development, 42(6), 918-927. https://doi.org/10.1111/cch.12380
Gavin, N. I., Gaynes, B. N., Lohr, K. N., Meltzer-Brody, S., Gartlehner, G., & Swinson, T. (2005). Perinatal depression: a systematic review of prevalence and incidence. Obstetrics & Gynecology, 106(5 Part 1), 1071-1083. https://doi.org/10.1097/01.AOG.0000183597.31630.db
Gelaye, B., Rondon, M. B., Araya, R., & Williams, M. A. (2016). Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. The Lancet Psychiatry, 3(10), 973-982. https://doi.org/10.1016/S2215-0366(16)30284-X
Guendelman, M. D., Ahmad, S., Meza, J. I., Owens, E. B., & Hinshaw, S. P. (2016). Childhood attention-deficit/hyperactivity disorder predicts intimate partner victimization in young women. Journal of abnormal child psychology, 44, 155-166. https://doi.org/10.1007/s10802-015-9984-z
Hayashi, W., Suzuki, H., Saga, N., Arai, G., Igarashi, R., Tokumasu, T., ... & Iwanami, A. (2019). Clinical characteristics of women with ADHD in Japan. Neuropsychiatric Disease and Treatment, 3367-3374. http://doi.org/10.2147/NDT.S232565
Henry, E., & Hill Jones, S. (2011). Experiences of older adult women diagnosed with attention deficit hyperactivity disorder. Journal of women & aging, 23(3), 246-262. https://doi-org.ejournals.um.edu.mt/10.1080/08952841.2011.589285
Hinshaw, S. P., Nguyen, P. T., O’Grady, S. M., & Rosenthal, E. A. (2022). Annual Research Review: Attention‐deficit/hyperactivity disorder in girls and women: underrepresentation, longitudinal processes, and key directions. Journal of Child Psychology and Psychiatry, 63(4), 484-496. https://doi-org.ejournals.um.edu.mt/10.1111/jcpp.13480
Holthe, M. E. G., & Langvik, E. (2017). The strives, struggles, and successes of women diagnosed with ADHD as adults. Sage Open, 7(1), 2158244017701799. https://doi.org/10.1177/2158244017701799
Hong, Q. N., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., ... & Pluye, P. (2018). The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for information, 34(4), 285-291. https://doi.org/10.3233/EFI-180221
Hylan, T. R., Sundell, K., & Judge, R. (1999). The impact of premenstrual symptomatology on functioning and treatment-seeking behavior: experience from the United States, United Kingdom, and France. Journal of women's health & gender-based medicine, 8(8), 1043-1052. https://doi.org/10.1089/jwh.1.1999.8.1043
Jones, H. A., Eddy, L. D., Rabinovitch, A. E., Snipes, D. J., Wilson, S. A., Parks, A. M., ... & Svikis, D. S. (2018). Attention‐deficit/hyperactivity disorder symptom clusters differentially predict prenatal health behaviors in pregnant women. Journal of Clinical Psychology, 74(4), 665-679. https://doi.org/10.1002/jclp.22538
Kakuszi, B., Bitter, I., & Czobor, P. (2018). Suicidal ideation in adult ADHD: Gender difference with a specific psychopathological profile. Comprehensive Psychiatry, 85, 23-29. https://doi.org/10.1016/j.comppsych.2018.06.003
Khan, K. S., Kunz, R., Kleijnen, J., & Antes, G. (2003). Five steps to conducting a systematic review. Journal of the royal society of medicine, 96(3), 118-121. https://doi.org/10.1177/014107680309600304
Klefsjö, U., Kantzer, A. K., Gillberg, C., & Billstedt, E. (2021). The road to diagnosis and treatment in girls and boys with ADHD–gender differences in the diagnostic process. Nordic journal of psychiatry, 75(4), 301-305. https://doi.org/10.1080/08039488.2020.1850859
Kok, F. M., Groen, Y., Fuermaier, A. B., & Tucha, O. (2016). Problematic peer functioning in girls with ADHD: A systematic literature review. PloS one, 11(11), e0165119. https://doi.org/10.1371/journal.pone.0165119
Kok, F. M., Groen, Y., Fuermaier, A. B., & Tucha, O. (2020). The female side of pharmacotherapy for ADHD—A systematic literature review. PLoS One, 15(9), e0239257. https://doi.org/10.1371/journal.pone.0239257
Kooij, S. J., Bejerot, S., Blackwell, A., Caci, H., Casas-Brugué, M., Carpentier, P. J., ... & Asherson, P. (2010). European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD. BMC psychiatry, 10, 1-24. https://link.springer.com/article/10.1186/1471-244X-10-67
Lassinantti, K., & Almqvist, A. L. (2021). ‘Mums Are Mums’: Negotiations of Parenthood Ideals Among Swedish Mothers with ADHD. Close Relations: Family, Kinship, and Beyond, 193-208. https://doi.org/10.1007/978-981-16-0792-9_12
Lizarondo, L., Stern, C., Carrier, J., Godfrey, C., Rieger, K., Salmond, S., ... & Loveday, H. (2020). Chapter 8: Mixed methods systematic reviews [internet]. JBI manual for evidence synthesis. SA, AUS: Joanna Briggs Institute. https://jbi-global-wiki.refined.site/space/MANUAL/4687380/Chapter+8%3A+Mixed+methods+ systematic+reviews
London, A. S., & Landes, S. D. (2021). Cohort change in the prevalence of ADHD among US adults: evidence of a gender-specific historical period effect. Journal of Attention Disorders, 25(6), 771-782. https://doi.org/10.1177/1087054719855689
Lynch, A., & Davison, K. (2022). Gendered expectations on the recognition of ADHD in young women and educational implications. Irish Educational Studies, 1-21. https://doi.org/10.1080/03323315.2022.2032264
Martin, J., Taylor, M. J., Rydell, M., Riglin, L., Eyre, O., Lu, Y., ... & Lichtenstein, P. (2018). Sex‐specific manifestation of genetic risk for attention deficit hyperactivity disorder in the general population. Journal of Child Psychology and Psychiatry, 59(8), 908-916. https://doi.org/10.1111/jcpp.12874
McKenzie, J. E., Brennan, S. E., Ryan, R. E., Thomson, H. J., Johnston, R. V., & Thomas, J. (2019). Defining the criteria for including studies and how they will be grouped for the synthesis. Cochrane handbook for systematic reviews of interventions, 33-65. https://doi.org/10.1002/9781119536604.ch3
Meyer, B. J., Stevenson, J., & Sonuga-Barke, E. J. (2020). Sex differences in the meaning of parent and teacher ratings of ADHD behaviors: an observational study. Journal of attention disorders, 24(13), 1847-1856. https://doi.org/10.1177/1087054717723988
Mowlem, F. D., Rosenqvist, M. A., Martin, J., Lichtenstein, P., Asherson, P., & Larsson, H. (2019). Sex differences in predicting ADHD clinical diagnosis and pharmacological treatment. European child & adolescent psychiatry, 28, 481-489. https://doi.org/10.1007/s00787-018-1211-3
Munn, Z., Porritt, K., Lockwood, C., Aromataris, E., & Pearson, A. (2014). Establishing confidence in the output of qualitative research synthesis: The ConQual approach. BMC medical research methodology, 14(1), 1-7. https://doi.org/10.1186/1471-2288-14-108
Nussbaum, N. L. (2012). ADHD and female specific concerns: a review of the literature and clinical implications. Journal of attention disorders, 16(2), 87-100. https://doi.org/10.1177/1087054711416909
Ostojic, D., & Miller, C. J. (2016). Association between pubertal onset and symptoms of ADHD in female university students. Journal of attention disorders, 20(9), 782-791. https://doi.org/10.1177/1087054714535249
Owens, E. B., Zalecki, C., Gillette, P., & Hinshaw, S. P. (2017). Girls with childhood ADHD as adults: Cross-domain outcomes by diagnostic persistence. Journal of consulting and clinical psychology, 85(7), 723. https://dx.doi.org/10.1037/ccp0000217
Park, J. L., & Johnston, C. (2019). Mothers’ attributions for positive and negative child behavior: Associations with mothers’ ADHD symptoms. Journal of Attention Disorders, 23(5), 475-486. https://doi.org/10.1177/1087054716669590
Pearson, A., White, H., Bath-Hextall, F., Salmond, S., Apostolo, J., & Kirkpatrick, P. (2015). A mixed-methods approach to systematic reviews. JBI Evidence Implementation, 13(3), 121-131. https://doi.org/10.1097/XEB.0000000000000052
Perez Algorta, G., Kragh, C. A., Arnold, L. E., Molina, B. S., Hinshaw, S. P., Swanson, J. M., ... & Jensen, P. S. (2018). Maternal ADHD symptoms, personality, and parenting stress: Differences between mothers of children with ADHD and mothers of comparison children. Journal of attention disorders, 22(13), 1266-1277. https://doi.org/10.1177/1087054714561290
Petticrew, M., Rehfuess, E., Noyes, J., Higgins, J. P., Mayhew, A., Pantoja, T., ... & Sowden, A. (2013). Synthesizing evidence on complex interventions: how meta-analytical, qualitative, and mixed-method approaches can contribute. Journal of clinical epidemiology, 66(11), 1230-1243. https://doi.org/10.1016/j.jclinepi.2013.06.005
Psychogiou, L., Daley, D. M., Thompson, M. J., & Sonuga-Barke, E. J. (2008). Do maternal attention-deficit/hyperactivity disorder symptoms exacerbate or ameliorate the negative effect of child attention-deficit/hyperactivity disorder symptoms on parenting? Development and psychopathology, 20(1), 121-137. https://doi.org/10.1017/S0954579408000060
Quinn, P. O. (2005). Treating adolescent girls and women with ADHD: Gender‐Specific issues. Journal of clinical psychology, 61(5), 579-587. https://doi-org.ejournals.um.edu.mt/10.1002/jclp.20121
Quinn, P. O. (2008). Attention-deficit/hyperactivity disorder and its comorbidities in women and girls: an evolving picture. Current psychiatry reports, 10(5), 419-423. https://doi.org/10.1007/s11920-008-0067-5
Quinn, P. O., & Madhoo, M. (2014). A review of attention-deficit/hyperactivity disorder in women and girls: Uncovering this hidden diagnosis. The primary care companion for CNS disorders, 16(3), 27250. https://doi.org/10.4088/pcc.13r01596
Ryan, C., Hesselgreaves, H., Wu, O., Paul, J., Dixon-Hughes, J., & Moss, J. G. (2018). Protocol for a systematic review and thematic synthesis of patient experiences of central venous access devices in anti-cancer treatment. Systematic reviews, 7(1), 1-7. https://doi.org/10.1186/s13643-018-0721-x
Skoglund, C., Kallner, H. K., Skalkidou, A., Wikström, A. K., Lundin, C., Hesselman, S., ... & Poromaa, I. S. (2019). Association of attention-deficit/hyperactivity disorder with teenage birth among women and girls in Sweden. JAMA network open, 2(10), e1912463-e1912463. https://doi.org/10.1001/jamanetworkopen.2019.12463
Snyder, J. A. (2015). The link between ADHD and the risk of sexual victimization among college women: Expanding the lifestyles/routine activities framework. Violence Against Women, 21(11), 1364-1384. https://doi.org/10.1177/1077801215593647
Solberg, B. S., Halmøy, A., Engeland, A., Igland, J., Haavik, J., & Klungsøyr, K. (2018). Gender differences in psychiatric comorbidity: a population‐based study of 40 000 adults with attention deficit hyperactivity disorder. Acta Psychiatrica Scandinavica, 137(3), 176-186. https://doi.org/10.1111/acps.12845
Stenner, P., O'Dell, L., & Davies, A. (2019). Adult women and ADHD: On the temporal dimensions of ADHD identities. Journal for the Theory of Social Behaviour, 49(2), 179-197. https://doi.org/10.1111/jtsb.12198
Surendran, I., Wijesinghe, K., & Johnson, J. (2022). Treatment of Attention Deficit Hyperactivity Disorder (ADHD) in Pregnant Women: A Systematic Review of Cohort Studies. BJPsych Open, 8(S1), S74-S74. https://doi.org/10.1192/bjo.2022.250
Szép, A., Skoluda, N., Schloß, S., Becker, K., Pauli-Pott, U., & Nater, U. M. (2021). The impact of preschool child and maternal attention-deficit/hyperactivity disorder (ADHD) symptoms on mothers’ perceived chronic stress and hair cortisol. Journal of Neural Transmission, 128, 1311-1324. https://doi.org/10.1007/s00702-021-02377-1
Terracciano, L., Brozek, J., Compalati, E., & Schünemann, H. (2010). GRADE system: new paradigm. Current opinion in allergy and clinical immunology, 10(4), 377-383. https://doi.org/10.1097/ACI.0b013e32833c148b
Thomas, J., & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC medical research methodology, 8(1), 1-10. https://doi.org/10.1186/1471-2288-8-45
Vildalen, V. U., Brevik, E. J., Haavik, J., & Lundervold, A. J. (2019). Females with ADHD report more severe symptoms than males on the adult ADHD self-report scale. Journal of attention disorders, 23(9), 959-967. https://doi.org/10.1177/1087054716659362
Waite, R. (2010). Women with ADHD: It is an explanation, not the excuse du jour. Perspectives in Psychiatric Care, 46(3), 182-196. https://doi-org.ejournals.um.edu.mt/10.1111/j.1744-6163.2010.00254.x
Wallin, K., Wallin Lundell, I., Hanberger, L., Alehagen, S., & Hultsjö, S. (2022). Self-experienced sexual and reproductive health in young women with Attention Deficit Hyperactivity Disorder: A qualitative interview study. BMC Women's Health, 22(1), 289. https://doi.org/10.1186/s12905-022-01867-y
Williamson, D., & Johnston, C. (2015). Gender differences in adults with attention-deficit/hyperactivity disorder: A narrative review. Clinical psychology review, 40, 15-27. https://doi-org.ejournals.um.edu.mt/10.1016/j.cpr.2015.05.005
Yoshimasu, K., Barbaresi, W. J., Colligan, R. C., Voigt, R. G., Killian, J. M., Weaver, A. L., & Katusic, S. K. (2018). Adults with persistent ADHD: Gender and psychiatric comorbidities—A population-based longitudinal study. Journal of attention disorders, 22(6), 535-546. https://doi.org/10.1177/1087054716676342
Young, S., Adamo, N., Ásgeirsdóttir, B. B., Branney, P., Beckett, M., Colley, W., ... & Woodhouse, E. (2020). Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/hyperactivity disorder in girls and women. BMC psychiatry, 20(1), 1-27. https://doi.org/10.1186/s12888-020-02707-9
Zaidman-Zait, A., & Shilo, I. (2021). Parental ADHD symptoms and inhibitory control in relation to parenting among mothers of children with and without ADHD. Journal of Attention Disorders, 25(3), 389-402. https://doi.org/10.1177/1087054718808063

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)