A Population-Based Study of Eating Disorders in Young Persons in Malta: Prevalence in Males Nearly Equals that in Females
Abstract
Objective: The objective of this study was to examine the prevalence of eating disorders and attitudes to food and eating for youths between 10 and 16 years of age, in order to aid in the diagnosis and treatment of eating disorders in young people through empirical research in a previously unexamined area.
Methods: The tool selected for this population-based study was the ChEAT, i.e. the Children’s Eating Attitudes Test. A representative cohort of 400, randomly sampled, young people aged 10-16, were asked all 26 questions of the ChEAT via telephone, while their parents/guardians were asked socio-demographic questions,
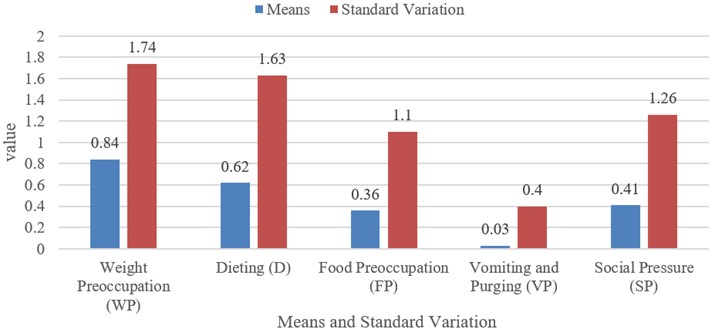
Results: 5.5% (2.25% M, 3.25% F) of the cohort scored at or above the cut-off of 20, indicating the presence of an eating disorder. No significant associations were found between disordered eating and socio-demographic data.
Conclusions: Findings indicate that males are catching up to females in eating disorder diagnoses. A male slightly higher mean ChEAT ≥20 could denote that disordered eating could be more acute for young men who are between 10 to 16 years old than it is for young women aged 10 to 16. The lack of significant association between the disordered eating and socio-demographic data could be a factor of the ages under examination in this study, and possibly these associations could arise at later ages.
References
American Psychiatric Association. (2013). The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5). https://doi.org/10.1176/appi.books.9780890425596
Austin, A., Flynn, M., Richards, K., Hodsoll, J., Duarte, T. A., Robinson, P., ... & Schmidt, U. (2021). Duration of untreated eating disorder and relationship to outcomes: A systematic review of the literature. European Eating Disorders Review, 29(3), 329-345. https://doi.org/10.1002/erv.2745
Azzopardi, A., Grech, A., & Cuff, A. (2020). Eating disorders amongst young persons in Malta: a nationally representative study of the prevalence and effect of eating disorders among young persons in Malta. Retrieved from https://www.um.edu.mt/library/oar/bitstream/123456789/76595/1/Eating_disorders_amongst_young%20_persons_in_Malta_a_nationally_representative_study_of_the_prevalence_and_effect_of_eating_disorders_among_young_persons_in_Malta_2020.pdf
Carta, M. G., Preti, A., Moro, M. F., Aguglia, E., Balestrieri, M., Caraci, F., ... & Bhugra, D. (2014). Eating disorders as a public health issue: prevalence and attributable impairment of quality of life in an Italian community sample. International Review of Psychiatry, 26(4), 486-492. https://doi.org/10.3109/09540261.2014.927753
Chiba H., Nagamitsu S., Sakurai R., Mukai T., Shintou H., 1 Koyanagi K., et al: Children's eating attitudes test: Reliability and validation in Japanese adolescents. Eating Behaviors, 23, 120-125. https://doi.org/10.1016/j.eatbeh.2016.09.001
Cooney M., Lieberman M., Guimond T. & Katzman D.K. (2018). Clinical and psychological features of children and adolescents diagnosed with avoidant/restrictive food intake disorder in a pediatric tertiary care eating disorder program: a descriptive study. Journal of Eating Disorders, 6,1-8. https://doi.org/10.1186/s40337-018-0193-3
Culbert K.M., Racine S.E., & Klump K.L. (2015). Research Review: What we have learned about the causes of eating disorders–a synthesis of sociocultural, psychological, and biological research. Journal of Child Psychology and Psychiatry, 56(11), 1141-1164. https://doi.org/10.1111/jcpp.12441
Eichstadt, M., Luzier, J., Cho, D., & Weisenmuller, C. (2020). Eating disorders in male athletes. Sports health, 12(4), 327-333. https://doi.org/10.1177/1941738120928991
Falzon Aquilina F., Grech A., Zerafa D., Agius M., & Voon V. (2015). 'DAR KENN GHAL SAHHTEK' - AN EATING DISORDER AND OBESITY SERVICE IN MALTA. Psychiatria Danubina, 27(suppl 1), 526-529. Retrieved from https://hrcak.srce.hr/file/384228
Fassino S. & Abbate-Daga G. (2013). Resistance to treatment in eating disorders: a critical challenge. BMC Psychiatry 13(1), 1-4. https://doi.org/10.1186/1471-244X-13-282
Ganson, K. T., Murray, S. B., & Nagata, J. M. (2021). Last word: A call to develop specific medical treatment guidelines for adolescent males with eating disorders. Eating Disorders, 29(4), 344-350. https://doi.org/10.1080/10640266.2019.1652474
Gorrell, S., & Murray, S. B. (2019). Eating disorders in males. Child and Adolescent Psychiatric Clinics, 28(4), 641-651. https://doi.org/10.1016/j.chc.2019.05.012
Grech, A. (2013). Eating disorders in Malta. Psychiatria Danubina, 25(suppl 2), 256-257.
Hoek, H. W. (2016). Review of the worldwide epidemiology of eating disorders. Current opinion in psychiatry, 29(6), 336-339. https://doi.org/10.1097/YCO.0000000000000282
Huang, Y., Wang, C., & Tong, L. (2023). The Reliability and Validation of the Children’s Eating Attitude Test among Chinese Samples. International Journal of Environmental Research and Public Health, 20(1), 738. https://doi.org/10.3390/ijerph20010738
Keski-Rahkonen, A., & Mustelin, L. (2016). Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Current opinion in psychiatry, 29(6), 340-345. https://doi.org/10.1097/YCO.0000000000000278
Legendre, M., Côté, M., Aimé, A., Brault, M. C., Dion, J., & Bégin, C. (2021). The children’s eating attitudes test: French validation of a short version. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 1-8. https://doi.org/10.1007/s40519-021-01158-9
Litmanen, J., Fröjd, S., Marttunen, M., Isomaa, R., & Kaltiala-Heino, R. (2017). Are eating disorders and their symptoms increasing in prevalence among adolescent population?. Nordic Journal of Psychiatry, 71(1), 61-66. https://doi.org/10.1080/08039488.2016.1224272
Lommi, S., Viljakainen, H. T., Weiderpass, E., & de Oliveira Figueiredo, R. A. (2020). Children’s Eating Attitudes Test (ChEAT): a validation study in Finnish children. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 25, 961-971. https://doi.org/10.1007/s40519-019-00712-w
Lyubov Matytsina, M. D., Greydanus, D. E., Babenko-Sorocopud, I. V., & Matytsina, L. (2014). Anorexia nervosa in adolescence: Current concepts of medical and psychological assessment and management. International Journal of Child and Adolescent Health, 7(3), 167.
Maloney, M. J., McGUIRE, J. B., & Daniels, S. R. (1988). Reliability testing of a children's version of the Eating Attitude Test. Journal of the American Academy of Child & Adolescent Psychiatry, 27(5), 541-543. https://doi.org/10.1097/00004583-198809000-00004
Mitchison, D., Hay, P., Slewa-Younan, S., & Mond, J. (2014). The changing demographic profile of eating disorder behaviors in the community. BMC Public Health, 14(1), 1-9. https://doi.org/10.1186/1471-2458-14-943
Mond, J., Hall, A., Bentley, C., Harrison, C., Gratwick‐Sarll, K., & Lewis, V. (2014). Eating‐disordered behavior in adolescent boys: Eating disorder examination questionnaire norms. International Journal of Eating Disorders, 47(4), 335-341. https://doi.org/10.1002/eat.22237
Murphy, T. J., Hwang, H., Kramer, M. S., Martin, R. M., Oken, E., & Yang, S. (2019). Assessment of eating attitudes and dieting behaviors in healthy children: Confirmatory factor analysis of the Children's Eating Attitudes Test. International Journal of Eating Disorders, 52(6), 669-680. https://doi.org/10.1002/eat.23062
Nagl, M., Jacobi, C., Paul, M., Beesdo-Baum, K., Höfler, M., Lieb, R., & Wittchen, H. U. (2016). Prevalence, incidence, and natural course of anorexia and bulimia nervosa among adolescents and young adults. European child & adolescent psychiatry, 25, 903-918. https://doi.org/10.1007/s00787-015-0808-z
Nardone, G., & Barbieri, R. B. (2010). Advanced Brief Strategic Therapy: An overview of interventions with eating disorders to exemplify how theory and practice work. European Journal of Psychotherapy and Counselling, 12(2), 113-127. https://doi.org/10.1080/13642537.2010.482743
NEDA: Eating disorders in men and boys (2022). National Eating Disorders Association. https://www.nationaleatingdisorders.org/learn/general-information/research-on-males
Ornstein, R. M., Essayli, J. H., Nicely, T. A., Masciulli, E., & Lane‐Loney, S. (2017). Treatment of avoidant/restrictive food intake disorder in a cohort of young patients in a partial hospitalization program for eating disorders. International Journal of Eating Disorders, 50(9), 1067-1074. https://doi.org/10.1002/eat.22737
Orsini, G. (2017). “Hunger hurts, but starving works”. The moral conversion to eating disorders. Culture, Medicine, and Psychiatry, 41(1), 111-141. https://doi.org/10.1007/s11013-016-9507-6
Pritchard, M. (2008). Disordered eating in undergraduates: Does gender role orientation influence men and women the same way? Sex Roles, 59, 282-289. https://doi.org/10.1007/s11199-008-9449-8
Raevuori, A., Keski-Rahkonen, A., & Hoek, H. W. (2014). A review of eating disorders in males. Current opinion in psychiatry, 27(6), 426-430. https://doi.org/10.1097/YCO.0000000000000113
Rolland, K., Farnill, D., & Griffiths, R. A. (1997). Body figure perceptions and eating attitudes among Australian schoolchildren aged 8 to 12 years. International Journal of Eating Disorders, 21(3), 273-278. https://doi.org/10.1002/(SICI)1098-108X(199704)21:3<273::AID-EAT7>3.0.CO;2-H
Sancho, C., Asorey, O., Arija, V., & Canals, J. (2005). Psychometric characteristics of the children's eating attitudes test in a Spanish sample. European Eating Disorders Review: The Professional Journal of the Eating Disorders Association, 13(5), 338-343. https://doi.org/10.1002/erv.643
Schmidt, U., Adan, R., Böhm, I., Campbell, I. C., Dingemans, A., Ehrlich, S., ... & Zipfel, S. (2016). Eating disorders: the big issue. The Lancet Psychiatry, 3(4), 313-315. https://doi.org/10.1016/S2215-0366(16)00081-X
Shu, C. Y., Limburg, K., Harris, C., McCormack, J., Hoiles, K. J., Hamilton, M. J., & Watson, H. J. (2015). Clinical presentation of eating disorders in young males at a tertiary setting. Journal of eating disorders, 3(1), 1-7. https://doi.org/10.1186/s40337-015-0075-x
Silén, Y., Sipilä, P. N., Raevuori, A., Mustelin, L., Marttunen, M., Kaprio, J., & Keski-Rahkonen, A. (2021). Detection, treatment, and course of eating disorders in Finland: A population-based study of adolescent and young adult females and males. European Eating Disorders Review, 29( 5), 720-732. https://doi.org/10.1002/erv.2838
Smink, F. R., Van Hoeken, D., & Hoek, H. W. (2012). Epidemiology of eating disorders: incidence, prevalence and mortality rates. Current psychiatry reports, 14(4), 406-414. https://doi.org/10.1007/s11920-012-0282-y
Smolak, L., & Levine, M. P. (1994). Psychometric properties of the children's eating attitudes test. International Journal of Eating Disorders, 16(3), 275-282. https://doi.org/10.1002/1098-108X(199411)16:3<275::AID-EAT2260160308>3.0.CO;2-U
Solmi, F., Hotopf, M., Hatch, S. L., Treasure, J., & Micali, N. (2016). Eating disorders in a multi-ethnic inner-city UK sample: prevalence, comorbidity and service use. Social Psychiatry and Psychiatric Epidemiology, 51, 369-381. https://doi.org/10.1007/s00127-015-1146-7
Stice, E., Becker, C. B., & Yokum, S. (2013). Eating disorder prevention: Current evidence‐base and future directions. International Journal of Eating Disorders, 46(5), 478-485. https://doi.org/10.1002/eat.22105
Stice, E., Marti, C. N., Shaw, H., & Jaconis, M. (2009). An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of abnormal psychology, 118(3), 587. https://doi.org/10.1037/a0016481
Strother, E., Lemberg, R., Stanford, S. C., & Turberville, D. (2013). Eating disorders in men: underdiagnosed, undertreated, and misunderstood. In Current findings on males with eating disorders (pp. 13-22). Routledge. https://doi.org/10.1080/10640266.2012.715512
Treasure, J., Claudino, A. M., & Zucker, N. (2010). 02/13. Eating Disorders. Lancet (London, England), 375(9714), 583-593. https://doi.org/10.1016/S0140-6736(09)61748-7
Treasure, J., Stein, D., & Maguire, S. (2015). Has the time come for a staging model to map the course of eating disorders from high risk to severe enduring illness? An examination of the evidence. Early intervention in psychiatry, 9(3), 173-184. https://doi.org/10.1111/eip.12170
van Hoeken, D., & Hoek, H. W. (2020). Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Current Opinion in Psychiatry, 33(6), 521. https://doi.org/10.1097/YCO.0000000000000641
Wing T. & Zhang M. (2015). Eating disorders. InnovAiT 8,685-691. https://doi.org/10.1177/1755738015594475
Wiseman, C. V., Peltzman, B., Halmi, K. A., & Sunday, S. R. (2004). Risk factors for eating disorders: Surprising similarities between middle school boys and girls. Eating Disorders, 12(4), 315-320. https://doi.org/10.1080/10640260490521398
Wong L, Goh LG & Ramachandran R (2022). Evolution of paediatric eating disorders in Singapore: a historical cohort study. Archives of Disease in Childhood, 107, 1046-1048. https://doi.org/10.1136/archdischild-2022-323925
Zimmerman, J., & Fisher, M. (2017). Avoidant/Restrictive Food Intake Disorder (ARFID). Current Problems in Pediatric and Adolescent Health Care, 47(4), 95-103. https://doi.org/10.1016/j.cppeds.2017.02.005

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright for this article is retained by the author(s), with first publication rights granted to the journal.
This is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).









1.png)